Subarachnoid hemorrhage is bleeding into the space between the brain and arachnoid membrane. It is most commonly caused by ruptured aneurysms and presents as sudden, severe headache often described as “the worst ever.”
Symptoms include neck stiffness, vomiting, photophobia, and loss of consciousness. Rapid deterioration can occur, making immediate hospital evaluation necessary.
CT and lumbar puncture confirm diagnosis, while angiography identifies the bleeding source. These imaging methods are essential for planning interventional or surgical treatment.
Treatment options include endovascular coiling or surgical clipping of aneurysms. Intensive monitoring and supportive therapy are critical to reduce rebleeding risk and improve survival.
| Disease Name | Subarachnoid Hemorrhage |
| Definition | A sudden hemorrhage occurring in the subarachnoid space between the surface of the brain and the meninges (membranes covering the brain), most often resulting from a ruptured aneurysm. |
| Symptoms | Sudden severe headache (often described as “the worst headache of my life”), nausea, vomiting, loss of consciousness, neck stiffness, photophobia, neurological deficits. |
| Causes | Ruptured cerebral aneurysm, arteriovenous malformations, head trauma, bleeding disorders, or, rarely, tumors. |
| Risk Factors | High blood pressure, smoking, family history of aneurysms, aging, excessive alcohol consumption, use of drugs such as cocaine. |
| Diagnostic Methods | Brain CT (computed tomography), CT angiography, lumbar puncture (if CT is inconclusive), MRI or MR angiography. |
| Treatment Methods | Intensive care support, stopping aneurysm rupture (surgical clipping or endovascular coiling), blood pressure control, neurological monitoring, pain and nausea management. |
| Complications | Cerebral edema, vasospasm (arterial narrowing), hydrocephalus, seizures, rebleeding, neurological disorders, permanent brain damage. |
| Surgical Requirement | If caused by an aneurysm, surgical clipping or coiling may be required to stop the bleeding. |
| Recovery Time | Depends on the degree of brain damage and treatment; may take weeks or months, and some patients may have permanent neurological sequelae. |
| Prevention Methods | Blood pressure control, avoiding smoking and excessive alcohol, healthy diet, regular exercise, aneurysm screening in high-risk individuals. |
Prof. Dr. Özgür KILIÇKESMEZ Prof. Dr. Kılıçkesmez holds the Turkish Radiology Competency Certificate, the Turkish Interventional Radiology Competency Certificate, Stroke Treatment Certification, and the European Board of Interventional Radiology (EBIR). In his academic career, he won the Siemens Radiology First Prize in 2008.
Interventional Radiology / Interventional Neuroradiology
What is Subarachnoid Hemorrhage?
Subarachnoid hemorrhage occurs in the subarachnoid space between the brain and surrounding tissues. The most common cause is the rupture of a cerebral artery aneurysm. This condition causes a sudden and extremely severe headache, which can be highly distressing for patients. Neck stiffness, nausea, and vomiting are also common symptoms. It can cause sudden loss of consciousness, leading to life-threatening complications. Subarachnoid hemorrhage is considered a high-mortality condition, and there is also a high risk of rebleeding and delayed cerebral ischemia. Therefore, early diagnosis and timely treatment are vital to prevent complications.
What Are the Causes of Subarachnoid Hemorrhage?
Subarachnoid hemorrhage is a serious medical condition that may have different causes. The most common cause, responsible for about 85% of cases, is the rupture of cerebral aneurysms—weak spots in the arteries of the brain that can burst and bleed. Other causes include congenital arteriovenous malformations (AVMs) that may rupture and bleed.
Head trauma is another frequent cause of subarachnoid hemorrhage. Blows to the head from accidents or falls can rupture vessels and cause bleeding. High blood pressure can weaken blood vessels and increase the risk of SAH by causing arterial walls to rupture. Chronic hypertension damages vessel walls, making them more susceptible to rupture.
Bleeding disorders, both inherited and acquired, can also increase the risk of SAH. Illicit drug use, particularly cocaine, can damage vessel integrity and raise the risk. In some cases, the exact cause is unclear, leading to idiopathic SAH. Such cases may suggest unknown risk factors.
Other medical conditions, such as cerebral amyloid angiopathy (especially in older adults), can also increase the risk by causing protein accumulation in cerebral vessels.
*We recommend filling out all fields so we can respond in the best possible way.
How Common Is Subarachnoid Hemorrhage?
The prevalence of subarachnoid hemorrhage (SAH) varies worldwide. Different populations show varying incidence rates, depending on geographic and demographic factors.
- On average, the global incidence is estimated at 6 to 10 cases per 100,000 person-years.
- In Japan, the annual SAH incidence is quite high, with 22.7 cases per 100,000.
- In Finland, it is reported at 19.7 per 100,000.
- In the USA and Australia, the incidence ranges from 6.5 to 8.6 per 100,000.
According to the Global Burden of Disease Study, there were 697,490 SAH cases worldwide in 2021—a 37% increase since 1990. However, the age-standardized incidence rate (ASIR) decreased from 11.69 per 100,000 in 1990 to 8.32 per 100,000 in 2021.
Demographically, SAH is more common in women, who make up 55–60% of cases. Most cases occur between ages 50 and 70, with a mean age of around 60. Individuals of Asian descent appear to have a higher risk, indicating significant geographic and ethnic differences.
How Does Subarachnoid Hemorrhage Develop?
The process begins with the rupture of blood vessels, leading to accumulation of blood between the brain and surrounding tissues. This usually results from aneurysm rupture, especially at arterial branch points with high hemodynamic stress. Aneurysms enlarge, weakening the vessel wall, and eventually rupture. Congenital vascular disorders such as AVMs can also cause bleeding. Head trauma and high blood pressure may also damage vessels and trigger bleeding.
The pathophysiological mechanism involves:
- Hemodynamic Stress: Increased blood flow stresses vessel walls and causes endothelial damage, contributing to aneurysm rupture.
- Inflammatory Response: Cytokines and metalloproteinases released after rupture further weaken the vessel wall and trigger inflammation.
- Blood Accumulation: Blood enters the subarachnoid space, rapidly increasing intracranial pressure and compressing brain tissue.
Clinically, symptoms usually start with a sudden, severe headache. Patients experience a “thunderclap” headache and may also have neck stiffness, nausea, and altered consciousness. The effect on cerebrospinal fluid circulation may lead to complications like vasospasm, delayed cerebral ischemia, and hydrocephalus.
What Are the Symptoms of Subarachnoid Hemorrhage?
Subarachnoid hemorrhage (SAH) presents with sudden and severe symptoms, the most common being a “thunderclap headache”—a very sudden and intense headache that peaks within minutes and signals a serious underlying problem.
Other symptoms include:
- Nausea and vomiting: Often occur with severe headache and are early signs of SAH.
- Neck stiffness: Meningeal irritation may cause neck rigidity or stiffness.
- Photophobia and phonophobia: Increased sensitivity to light and sound is common, causing patients to avoid such stimuli.
- Altered consciousness: Depending on the severity, patients may experience confusion, lethargy, or even coma in severe cases.
- Seizures: Can occur acutely at the onset or during the early stage of hemorrhage.
- Focal neurological deficits: Patients may have weakness, numbness, speech difficulties, or vision loss, mimicking stroke symptoms.
Less commonly, syncope (fainting) or dizziness may occur. Some patients may report “warning headaches” lasting for days before a major hemorrhage, possibly indicating a minor leak.
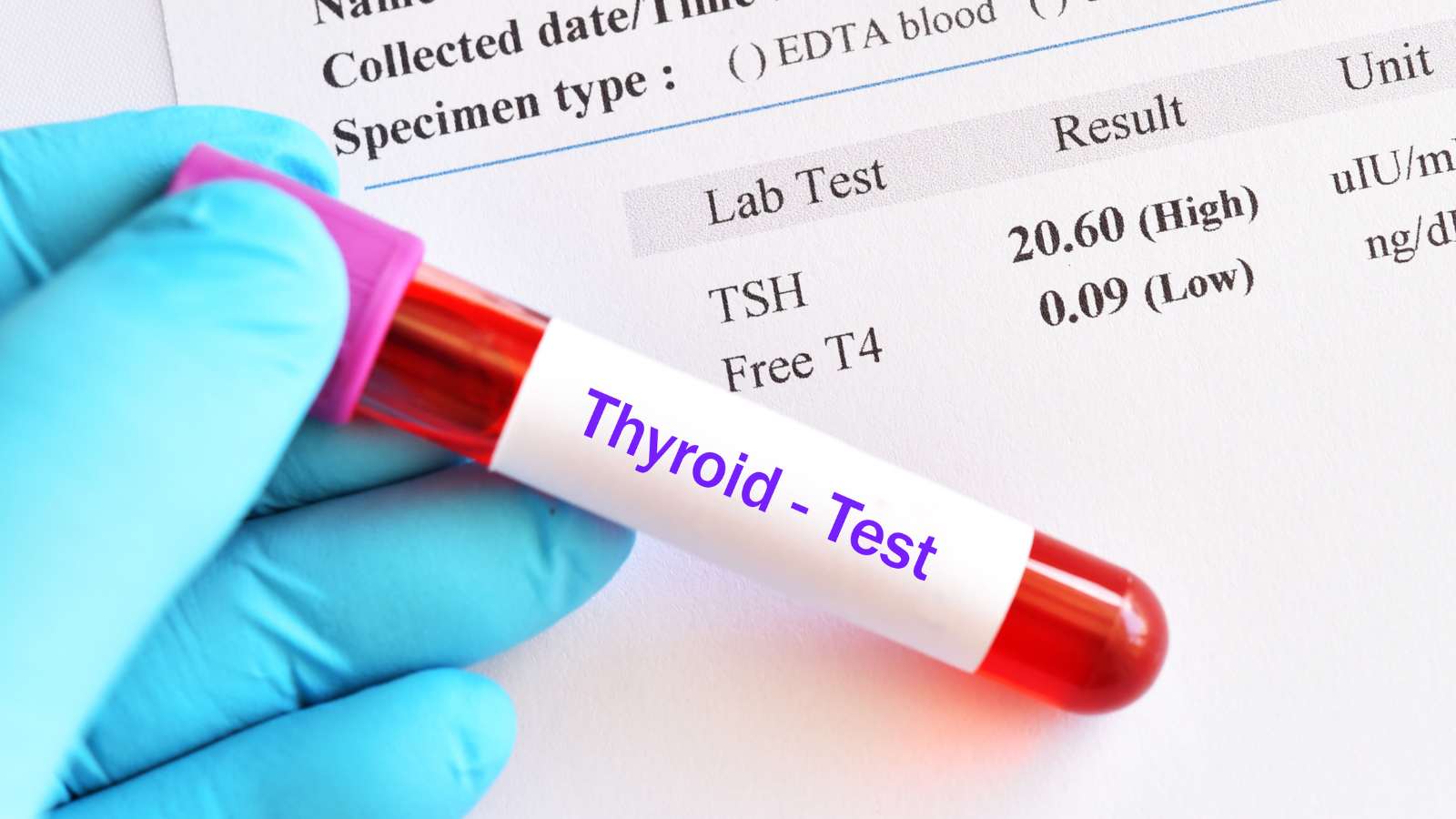
How Is Subarachnoid Hemorrhage Diagnosed?
The diagnosis of SAH often begins with the patient’s report of a “thunderclap headache.” Physicians then use imaging and laboratory tests for confirmation. Non-contrast CT is performed first; this method is highly sensitive for detecting bleeding within the first 6 hours. After that, CT sensitivity declines.
If CT is negative but clinical suspicion remains, lumbar puncture (LP) is performed. LP is highly effective for detecting breakdown products of blood in cerebrospinal fluid, especially when more than 6 hours have passed since symptom onset.
CT angiography (CTA) is performed in confirmed SAH cases to visualize aneurysms. CTA is fast, noninvasive, and detects aneurysms larger than 3–4 mm with 96–99% sensitivity.
If CTA does not detect an aneurysm, catheter angiography is used as the gold standard for detailed imaging. This is preferred when CTA is negative but SAH is confirmed, especially in non-traumatic cases.
Severity grading scales play an important role in diagnosis. The following are used to assess SAH severity and predict outcomes:
- WFNS Scale: Based on the Glasgow Coma Scale and motor deficits.
- Hunt and Hess Scale: Assesses mortality risk.
- Modified Fisher Scale: Predicts complications based on initial CT findings.
How Is Subarachnoid Hemorrhage Treated?
Interventional radiology, particularly endovascular techniques, plays a critical role in the treatment of subarachnoid hemorrhage. These methods are used for both aneurysm repair and the management of complications such as vasospasm. Common approaches include endovascular coiling, flow-diverting devices, and vasospasm management:
- Endovascular Coiling: The most common technique for treating aneurysmal SAH. A catheter is guided through the femoral artery to the brain aneurysm, and platinum coils are placed within the aneurysm to promote clotting. For complex aneurysms, advanced techniques like balloon-assisted or stent-assisted coiling may be used, but these require antiplatelet therapy, which can carry additional risks.
- Flow-Diverting Devices: Used for large or complex aneurysms, these stents redirect blood flow away from the aneurysm, supporting vessel healing. Usually reserved for unruptured aneurysms or after stabilization, their use is limited by the need for antiplatelet therapy.
- Vasospasm Management: Vasospasm after SAH increases the risk of delayed stroke. Interventional radiologists may infuse vasodilator drugs intra-arterially at the site of spasm. If this is not effective, balloon angioplasty can be performed to widen narrowed vessels, though this carries risk, especially in small arteries.
What Are the Risk Factors for Subarachnoid Hemorrhage?
Risk factors for SAH include both modifiable and non-modifiable elements, affecting lifestyle, genetics, and the environment. Chronic hypertension is the most important modifiable risk factor, as it increases the likelihood of intracranial aneurysm formation and rupture by weakening vessel walls.
Smoking is another major risk factor, promoting aneurysm formation through vascular wall damage. Genetic predisposition also increases risk—individuals with a family history of SAH or aneurysm have higher susceptibility, possibly due to vascular wall polymorphisms. Age is significant as well, with risk increasing sharply after age 50, especially between ages 50 and 60.
Excessive alcohol consumption is another clear risk, as it damages vessel walls and raises blood pressure. Similarly, stimulant drugs like cocaine can cause sudden blood pressure spikes and dramatically increase risk, even in younger individuals. Hormonal changes, especially reduced estrogen in postmenopausal women, can also affect vascular health and SAH risk.
The microbiome may also play a role; certain imbalances may contribute to SAH development, according to recent research. Other specific risk factors include:
- Hypertension
- Smoking
- Genetic predisposition
- Female gender
- Age
- Alcohol consumption
- Cocaine and illicit drug use
- Microbiome factors
- Previous aneurysm history
- Certain comorbidities (e.g., polycystic kidney disease, Ehlers-Danlos syndrome, Marfan syndrome)
When Can Subarachnoid Hemorrhage Be Treated?
Treatment of subarachnoid hemorrhage should be planned quickly, depending on the patient’s condition and the severity of bleeding. Early intervention after bleeding is essential to prevent rebleeding and reduce mortality, especially within the first 24 hours. Stabilizing the patient and initiating appropriate therapy as soon as possible is vital.
Treatment choices and timing depend on the following factors:
- Location and morphology of the aneurysm: Surgical clipping or coiling is selected based on aneurysm size and location; more complex cases may require stent-assisted coiling.
- Aneurysm status: Early intervention is required for ruptured aneurysms to prevent rebleeding; unruptured aneurysms carry different risks.
- Patient health: Age, comorbidities, and neurological status are considered when determining the best timing for intervention.
To reduce the risk of vasospasm, which often occurs 3–14 days after hemorrhage, intra-arterial vasodilators or balloon angioplasty may be applied during this period to minimize the risk of cerebral ischemia. Early intervention greatly reduces the risks of death and disability, so the timing of therapy should be decided on an individual basis.
When Can Subarachnoid Hemorrhage Not Be Treated?
Treatment of subarachnoid hemorrhage may not be feasible in some patients due to specific risk factors. Some situations may reduce the safety and effectiveness of interventional radiology procedures:
- Bleeding disorders or anticoagulant therapy: Clotting disorders must be corrected before treatment to avoid severe intraoperative bleeding complications.
- Severe vasospasm: Severe vasospasm after hemorrhage can prevent successful endovascular treatment; in such cases, medical therapy to reduce spasm is preferred first.
- Aneurysm morphology: Wide-necked or complex aneurysms, and aneurysms in the posterior circulation, may make procedures like coiling more difficult and risky.
- Uncontrolled hypertension: Blood pressure must be reduced before treatment; uncontrolled hypertension increases bleeding risk during or after procedures.
- Severe hydrocephalus or mass effect: Neurosurgical procedures such as external drainage may be needed before interventional treatment if these conditions are present.
- High risk of delayed cerebral ischemia: If risk is high, medical therapy is prioritized and extra precautions are taken if endovascular intervention is needed.
What Is the Recovery Process After Subarachnoid Hemorrhage Treatment?
The recovery process after subarachnoid hemorrhage treatment consists of several stages, with complication management being particularly important. Neurocognitive and psychological impacts play a key role—memory issues, executive dysfunction, and depression are common and may increase long-term rehabilitation needs. Anxiety and PTSD can also complicate recovery.
Vasospasm and delayed cerebral ischemia are among the most common complications during treatment. Vasospasm narrows brain arteries and can cause ischemic damage. Management includes:
- Administration of calcium channel blockers
- Continuous monitoring through imaging
- Angioplasty or intra-arterial vasodilator infusion as needed
Hydrocephalus, another major complication, can develop if blood blocks cerebrospinal fluid pathways. It is managed by temporary external drainage or permanent shunt placement.
Physical rehabilitation and neurological monitoring are essential to address motor deficits and neurological dysfunctions. Physical and occupational therapy are needed, with early mobilization encouraged but always balancing against complication risks.
How Can Subarachnoid Hemorrhage Be Prevented?
Several strategies can help prevent subarachnoid hemorrhage. Hypertension is the most important modifiable risk factor, so blood pressure control is critical. Lifestyle changes can significantly lower SAH risk, including:
- Regular exercise
- Low-sodium diet
- Smoking cessation
- Reducing alcohol intake
High-risk individuals should be screened regularly with imaging (MRI or CT angiography) for aneurysm detection. Unruptured aneurysms should be monitored using scoring systems. Conditions such as diabetes and high cholesterol should also be controlled with medication.
Effective prevention begins with risk factor management. Careful monitoring and surgical intervention when necessary are vital to reduce the risk of rupture and subsequent SAH. These measures are the foundation for preventing future SAH events, potentially reducing both mortality and disability rates.

Girişimsel Radyoloji ve Nöroradyoloji Uzmanı Prof. Dr. Özgür Kılıçkesmez, 1997 yılında Cerrahpaşa Tıp Fakültesi’nden mezun oldu. Uzmanlık eğitimini İstanbul Eğitim ve Araştırma Hastanesi’nde tamamladı. Londra’da girişimsel radyoloji ve onkoloji alanında eğitim aldı. İstanbul Çam ve Sakura Şehir Hastanesi’nde girişimsel radyoloji bölümünü kurdu ve 2020 yılında profesör oldu. Çok sayıda uluslararası ödül ve sertifikaya sahip olan Kılıçkesmez’in 150’den fazla bilimsel yayını bulunmakta ve 1500’den fazla atıf almıştır. Halen Medicana Ataköy Hastanesi’nde görev yapmaktadır.







Vaka Örnekleri