Parathormone (PTH) is a hormone secreted by the parathyroid glands that regulates calcium and phosphorus balance. Abnormal PTH levels can indicate endocrine or metabolic disorders.
High parathormone levels are commonly seen in hyperparathyroidism, kidney failure, or vitamin D deficiency. Symptoms may include bone pain, fatigue, kidney stones, and gastrointestinal disturbances.
Low parathormone levels occur in hypoparathyroidism, often following thyroid or parathyroid surgery. Patients may experience muscle cramps, tingling, or seizures due to low calcium levels.
PTH testing is essential for evaluating calcium metabolism disorders. Accurate interpretation helps guide treatment, including supplementation, surgery, or pharmacological therapy.
| Hormone Name | Parathyroid Hormone (PTH) |
| Definition | A hormone secreted by the parathyroid glands that plays a key role in the body’s balance of calcium, phosphorus, and vitamin D. |
| Functions | Increases blood calcium levels; stimulates calcium release from bones, enhances calcium reabsorption in the kidneys, and supports vitamin D activation. |
| Normal Range | Varies by laboratory, but generally considered to be 10–65 pg/mL. |
| Causes of High PTH | Primary hyperparathyroidism (tumor or enlargement of the parathyroid gland), vitamin D deficiency, chronic kidney failure, secondary hyperparathyroidism. |
| Causes of Low PTH | Hypoparathyroidism (underactive parathyroid gland), excessively high blood calcium, surgical removal of the parathyroid glands. |
| Symptoms of High PTH | Bone weakness, increased fracture risk, kidney stones, fatigue, muscle weakness, joint and bone pain. |
| Symptoms of Low PTH | Muscle cramps, tingling or numbness (especially in hands, feet, and face), muscle spasms, seizures, dry skin. |
| Diagnostic Methods | Blood tests to measure PTH, calcium, phosphorus, and vitamin D levels; kidney function tests and thyroid ultrasound for high PTH. |
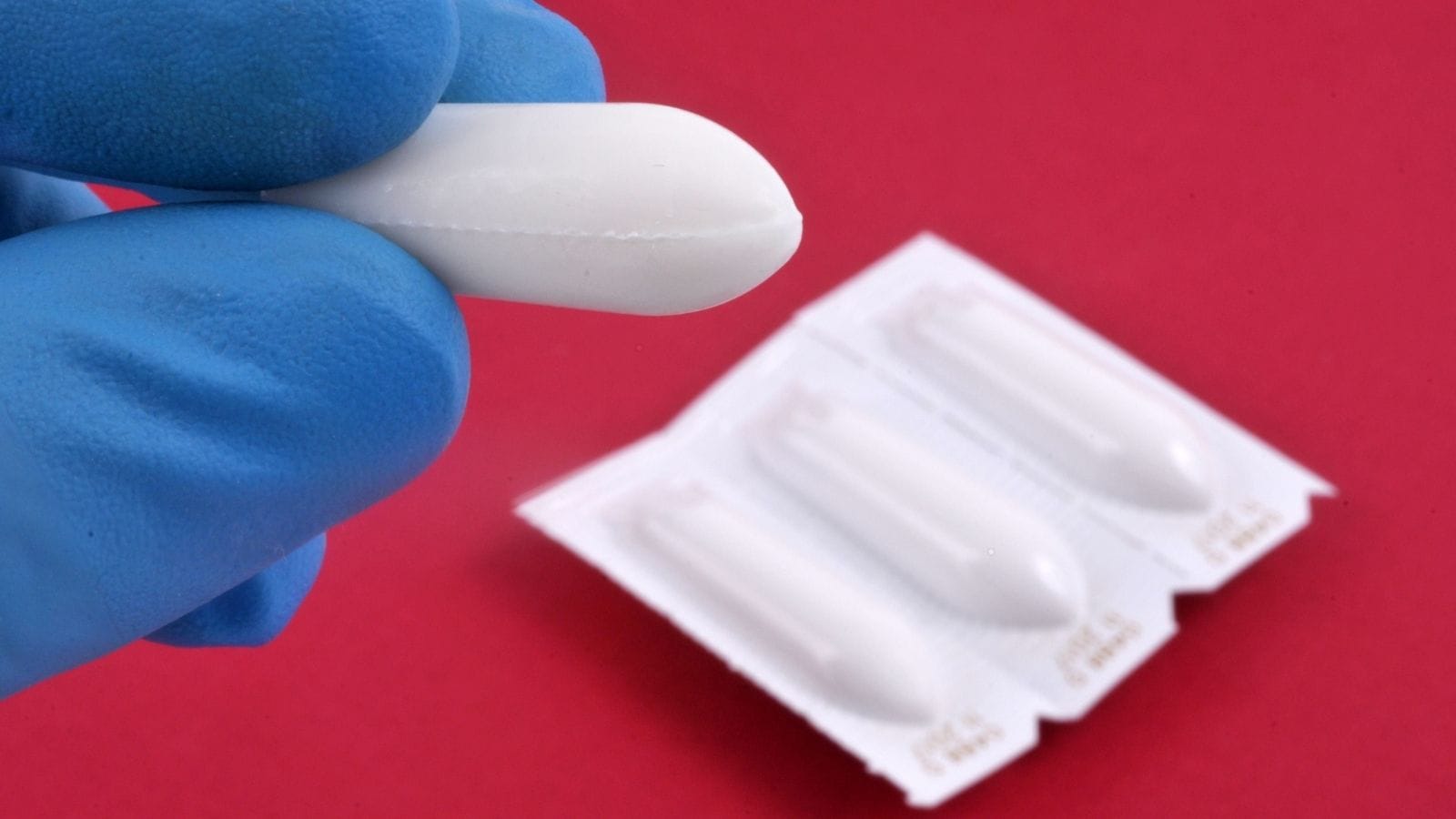
| Treatment Methods | High PTH: Surgery (parathyroidectomy), medication (calcimimetics, vitamin D); Low PTH: Calcium and vitamin D supplementation, synthetic PTH therapy if needed. Parathyroid adenomas can be treated with RF and microwave ablation or embolization. |
| Complications | Prolonged high PTH can lead to osteoporosis, kidney stones, and increased risk of cardiovascular disease. |
| Follow-up and Monitoring | Regular measurement of PTH, calcium, and vitamin D levels; monitoring of kidney and bone health. |
| Associated Diseases | Hyperparathyroidism, hypoparathyroidism, osteoporosis, chronic kidney disease, vitamin D deficiency. |
Prof. Dr. Özgür KILIÇKESMEZ Prof. Dr. Kılıçkesmez holds the Turkish Radiology Competency Certificate, the Turkish Interventional Radiology Competency Certificate, Stroke Treatment Certification, and the European Board of Interventional Radiology (EBIR). In his academic career, he won the Siemens Radiology First Prize in 2008.
Interventional Radiology / Interventional Neuroradiology
What Is PTH (Parathyroid Hormone)?
Parathyroid hormone (PTH) is a key hormone in maintaining the balance of calcium and phosphate in the body. Secreted by the parathyroid glands, PTH increases calcium levels by promoting the release of calcium from bones. It also enhances calcium reabsorption in the kidneys and activates vitamin D, increasing calcium absorption from the intestines. Additionally, to maintain phosphate balance, PTH reduces phosphate reabsorption in the kidneys, increasing its excretion. All these processes are vital for maintaining healthy bone structure and muscle function. Imbalances in PTH can lead to serious metabolic issues and threaten bone health, so its proper regulation is essential.
What Are the Causes of High PTH Levels?
Elevated parathyroid hormone (PTH) levels generally indicate various health problems and are categorized into three main types: primary, secondary, and tertiary hyperparathyroidism.
Primary hyperparathyroidism occurs when one or more parathyroid glands are overactive. The most common cause is a benign tumor called an adenoma. Parathyroid gland hyperplasia (enlargement) or, rarely, parathyroid cancer can also cause primary hyperparathyroidism.
Secondary hyperparathyroidism is a compensatory response to low calcium or vitamin D levels. Chronic kidney disease is the most common cause. Because the kidneys cannot convert vitamin D to its active form and cannot maintain calcium balance, PTH production increases. Vitamin D deficiency or gastrointestinal disorders that reduce calcium absorption can also trigger this condition.
Tertiary hyperparathyroidism develops as a result of long-standing secondary hyperparathyroidism. In this situation, the parathyroid glands continue to produce excess PTH even after the initial cause has been resolved.
Other causes of high PTH include certain medications and, rarely, the presence of macro-PTH. Lithium and thiazide diuretics, in particular, can affect calcium balance and raise PTH levels.
How Common Is High PTH?
The prevalence of elevated parathyroid hormone (PTH) is mostly associated with primary hyperparathyroidism (PHPT) and varies by age, gender, and race. PHPT is the most common cause of high PTH and is especially frequent in older individuals, with a marked increase after age 50. Women, especially postmenopausal, are at higher risk than men.
- Elevated PTH is more common in individuals over age 50.
- Postmenopausal women are 2 to 3 times more likely than men to have high PTH.
- PTH elevation can be seen in up to 2% of women over 60.
Racial differences are also important. Research shows that African-American women have higher rates of elevated PTH. African-American women aged 70–79 have higher rates of PHPT than other racial groups.
- African-American women are at higher risk than White, Asian, and Hispanic women.
Socioeconomic status and education level are also associated with PTH elevation. Individuals with lower education, lower socioeconomic status, and unmarried people have a higher likelihood of high PTH.
Secondary hyperparathyroidism is another cause of elevated PTH and is most often related to chronic kidney disease, particularly in older adults and those with renal problems.
*We recommend filling out all fields so we can respond in the best possible way.
How Is PTH Produced?
Parathyroid hormone (PTH) is produced through a complex biosynthetic process in the parathyroid glands. Initially, a precursor molecule called preproPTH (115 amino acids) is produced in the ribosomes of the chief cells of the parathyroid glands. A signal sequence at the N-terminus of preproPTH directs the molecule to the endoplasmic reticulum.
After entering the endoplasmic reticulum, the signal sequence is removed, converting preproPTH to proPTH (90 amino acids). ProPTH is then transported to the Golgi apparatus. There, further processing removes an additional sequence at the N-terminus, resulting in mature PTH (84 amino acids). Mature PTH is packaged into secretory vesicles and stored in the parathyroid glands.
PTH secretion is regulated by the calcium-sensing receptor (CaSR) on the surface of parathyroid cells, which is sensitive to serum calcium levels. Low calcium decreases CaSR activity, triggering the release of PTH into the bloodstream. High calcium suppresses PTH secretion.
Vitamin D and phosphate levels also affect PTH production:
- 1,25-dihydroxyvitamin D suppresses PTH gene transcription.
- Increased phosphate levels stimulate PTH synthesis.
What Are the Symptoms of High PTH?
Elevated parathyroid hormone (PTH) disrupts the body’s calcium and phosphate balance, causing various symptoms that may progress over time or be mistaken for other conditions. Paying attention to symptoms is important for proper diagnosis.
On the skeletal system, high PTH weakens bones and makes them more fragile, leading to osteoporosis and increased fracture risk. Rarely, it can cause a bone disease called osteitis fibrosa cystica.
In the kidneys, there is a higher risk of kidney stones and calcium deposits, as excess blood calcium is excreted in the urine.
Gastrointestinal effects include nausea, constipation, and abdominal pain, often due to the effect of calcium imbalance on smooth muscles.
Mental and cognitive issues such as depression, anxiety, and memory problems may also be seen. Severe cases can involve confusion.
Muscle weakness and joint pain can make daily life difficult, as disrupted calcium metabolism directly affects muscle function.
Finally, in the cardiovascular system, high PTH increases the risk of hypertension and heart disease, and can cause vascular calcification over time.
How Is High PTH Diagnosed?
Diagnosing high parathyroid hormone (PTH) is based on a thorough evaluation of underlying causes, taking into account blood parameters such as calcium, phosphate, and vitamin D levels. The distinction between primary and secondary hyperparathyroidism is usually made. Primary hyperparathyroidism is characterized by hypercalcemia and is most often due to parathyroid adenomas.
Secondary hyperparathyroidism is usually caused by chronic kidney disease or vitamin D deficiency. In this case, calcium may be low or normal while PTH is high. Serum calcium should be adjusted for albumin levels. Kidney function must also be evaluated, as chronic kidney disease is often associated with secondary hyperparathyroidism.
Laboratory tests used in diagnosis include:
- Serum calcium and phosphate measurements
- Vitamin D and creatinine levels
- Kidney function tests
Imaging methods, especially sestamibi scan or ultrasound, are used to detect parathyroid adenomas. In patients at risk for tertiary hyperparathyroidism, further tests can be performed to evaluate if high PTH is persistent.
Bone mineral density measurements (DXA) are used to monitor bone health in cases of long-term high PTH. These tests help detect complications such as osteoporosis.
How Is High PTH Treated?
In hyperparathyroidism, interventional radiology plays a key role when surgery is risky or not suitable for the patient. These minimally invasive techniques are used to control high parathyroid hormone (PTH) levels and provide alternatives to surgery. Treatment options focus on destroying the overactive parathyroid glands.
- Radiofrequency Ablation (RFA): Uses radiofrequency waves to heat and destroy abnormal parathyroid tissue. It has been shown to be effective in both primary and secondary hyperparathyroidism and is a safe option for patients not suitable for general anesthesia.
- Microwave Ablation (MWA): Uses heat to destroy overactive parathyroid glands and safely lowers PTH levels, especially for patients who cannot have surgery.
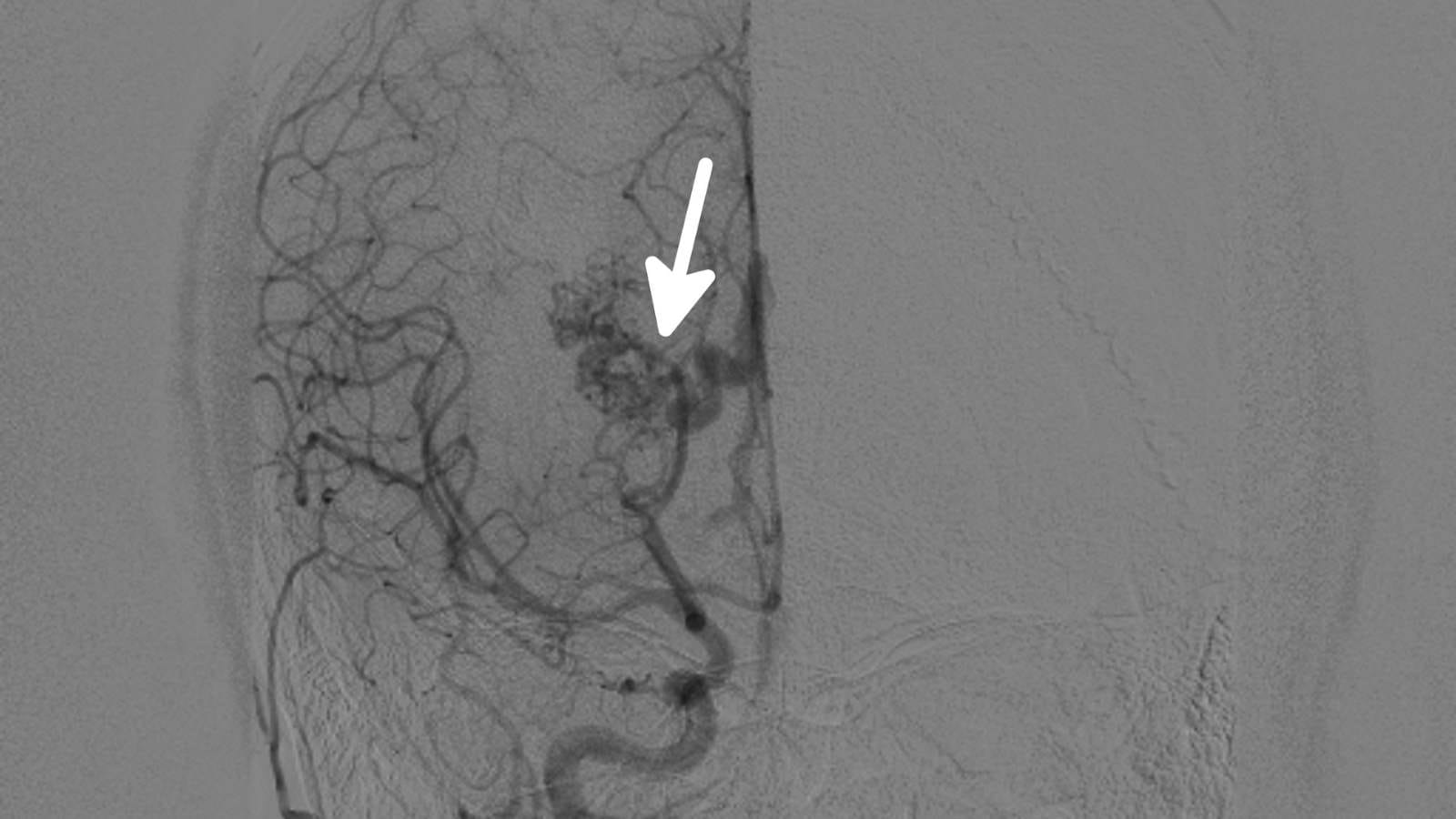
- Parathyroid Embolization: If the parathyroid tissue is in a location not accessible by ablation or surgery, blood supply to the tumor can be stopped by angiography to stabilize the clinical situation.
- High-Intensity Focused Ultrasound (HIFU): A non-invasive technique that uses focused ultrasound waves to thermally destroy parathyroid tissue. It is especially used in patients with kidney failure and effectively lowers PTH levels.
These interventional methods are especially strong alternatives to surgery in cases of recurrent hyperparathyroidism and in patients with multiple disease sites. Early results show these treatments are both safe and effective.
What Are the Risk Factors for PTH Abnormalities?
Elevated parathyroid hormone (PTH) levels can be affected by many risk factors and may arise in different situations, including both metabolic and environmental causes.
Vitamin D deficiency is a major contributor to high PTH. Lack of vitamin D reduces intestinal calcium absorption, forcing the parathyroid glands to produce more hormone. Chronic kidney disease is also a common reason for high PTH, as impaired kidney function prevents activation of vitamin D and proper calcium balance.
Primary hyperparathyroidism arises from abnormalities of the parathyroid glands themselves. Adenomas, hyperplasia, or cancer can cause unregulated hormone production. Lithium therapy is also associated with elevated PTH, thought to act on calcium-sensing receptors in the glands.
Older adults, especially postmenopausal women, can develop high PTH due to changes in calcium metabolism. Obesity and metabolic syndrome may also contribute to increased hormone levels. Diet and lifestyle factors play a role; low calcium intake and high phosphate consumption can increase PTH. Finally, hypertension and cardiovascular risk are also related to PTH levels.
When Can High PTH Be Treated?
Treatment of elevated parathyroid hormone (PTH) levels becomes especially relevant when surgery is not possible or has failed. In hyperparathyroidism, interventional radiology techniques offer a minimally invasive approach and are an important alternative for patients who are not surgical candidates. Common causes of high PTH include parathyroid adenomas, hyperplasia, or secondary hyperparathyroidism due to chronic kidney disease.
Some commonly used interventional radiology techniques include:
- Percutaneous Ablation: Performed under ultrasound guidance and includes techniques such as radiofrequency ablation (RFA), microwave ablation, and laser thermal ablation. Used mainly in patients not suitable for surgery and effective in suppressing parathyroid function.
- Percutaneous Ethanol Injection (PEI): Used for small, benign-appearing adenomas when surgery is risky. The aim is to destroy parathyroid tissue with ethanol ablation.
- Selective Venous Sampling (SVS): An invasive technique to directly measure PTH levels for accurate localization of suspicious parathyroid tissue, especially in recurrent cases.
- High-Intensity Focused Ultrasound (HIFU): A non-invasive method that targets parathyroid tissue with ultrasound energy and is effective, especially in managing secondary hyperparathyroidism.
When Can PTH Treatment Not Be Performed?
Interventional radiology procedures used to treat high parathyroid hormone (PTH) are not suitable in certain situations. The main factors limiting these procedures depend on the patient’s overall condition and the requirements of the procedure.
Patients with bleeding disorders are not suitable candidates. Especially those with coagulopathy, thrombocytopenia, or those on anticoagulant therapy have increased bleeding risk. For these patients, interventional procedures are contraindicated as they cannot be performed safely.
These procedures are also not preferred in patients with severe chronic kidney disease, as it may be difficult to control calcium levels, increasing the risk of complications. End-stage renal disease may present additional issues.
- Bleeding disorders: Not performed in patients with high bleeding risk.
- Severe chronic kidney disease: Not suitable for patients with advanced renal failure.
- Infection: Not performed in patients with active infections due to risk of spread.
- Liver or systemic disease: Not suitable for patients with severe liver failure.
- Tumor involvement: Patients with malignant parathyroid adenoma are at higher risk.
- Non-responsive parathyroid hyperplasia: May be difficult to effectively target hyperplastic glands.
What Is the Recovery Process After PTH Treatment?
The recovery process after treatment for elevated parathyroid hormone (PTH) levels allows patients to return to normal life quickly. Most patients experience minimal discomfort after the procedure, which can usually be managed with simple painkillers. Most are discharged on the same day or within 24 hours. Early mobilization is encouraged, and monitoring vital signs and serum calcium levels is crucial.
Important points in the recovery period include:
- Regular monitoring of serum calcium and PTH levels.
- Calcium supplementation may be required due to the risk of hypocalcemia.
- Fluctuations in calcium levels may occur in the first days.
In the long-term, patients’ conditions should be closely monitored to evaluate the effectiveness of ablation. Repeat ablation procedures may be needed, but complication risk is lower than with open surgery. Still, hematoma or infection may rarely occur, and the risk of hypoparathyroidism should be considered. Overall health should be monitored continuously and necessary precautions taken.
How Can PTH Level Disorders Be Prevented?
Preventing PTH disorders relies on several important strategies. First, vitamin D levels should be kept within the optimal range, as deficiency is a major cause of secondary hyperparathyroidism. Adequate vitamin D intake can lower PTH levels. Calcium balance is also essential—maintaining normal calcium levels helps control PTH secretion. Calcium supplementation may be beneficial for people at risk of deficiency or malabsorption.
Phosphate levels should also be monitored, especially in those with chronic kidney disease. Phosphate retention increases PTH secretion. Magnesium is another important factor; low magnesium impairs PTH regulation and bone health. Adequate magnesium intake can improve both PTH levels and bone health.
Finally, lifestyle changes are important. Regular physical activity, maintaining a healthy body weight, and avoiding smoking can help balance PTH levels. These changes are effective for preventing metabolic issues related to high PTH.
Frequently Asked Questions

What happens if parathyroid hormone is high?
High parathyroid hormone (PTH) levels result in a condition called hyperparathyroidism. This increases calcium release from bones, raises calcium absorption from the gut, and decreases calcium excretion from the kidneys, leading to elevated blood calcium. This causes symptoms such as fatigue, muscle weakness, nausea, vomiting, constipation, increased thirst, frequent urination, depression, and confusion. Long-term high calcium can lead to kidney stones, osteoporosis, and heart problems.
Why is the parathyroid hormone test done?
A PTH test is done to assess parathyroid gland function and diagnose conditions affecting calcium metabolism. It helps determine the causes of abnormal calcium levels, such as hyperparathyroidism or hypoparathyroidism, as well as chronic kidney disease and osteoporosis. It is also used to monitor the effectiveness of treatment.
What does parathyroid hormone deficiency cause?
PTH deficiency results in hypoparathyroidism, leading to low blood calcium (hypocalcemia) and high phosphate (hyperphosphatemia). This causes muscle cramps, involuntary spasms (tetany), seizures, and heart rhythm disturbances. Long-term hypocalcemia can lead to cataracts, dental problems, and brain calcifications, causing neurological issues. Dry skin, brittle nails, and hair loss may also occur. Chronic effects include kidney dysfunction, kidney stones, and decreased bone mineral density.
Is high parathyroid hormone cancer?
High parathyroid hormone (PTH) is usually due to primary hyperparathyroidism, most often caused by benign parathyroid adenomas. Rarely, high PTH levels may indicate parathyroid cancer, a malignant condition of the glands. Parathyroid cancer accounts for less than 1% of cases. Thus, high PTH is usually a sign of hyperparathyroidism, not cancer.
How is high parathyroid hormone reduced?
High PTH levels are most effectively reduced by surgical removal of the overactive gland (parathyroidectomy), especially in primary hyperparathyroidism. In secondary hyperparathyroidism, it is important to correct the underlying problem, such as vitamin D deficiency or chronic kidney disease. Vitamin D supplements, phosphate binders, or drugs like cinacalcet can be used. Regular monitoring and personalized treatment are vital.
At what PTH level is surgery needed?
Surgery is recommended for primary hyperparathyroidism when symptoms such as kidney stones, osteoporosis, or neuromuscular problems occur. If there are no symptoms, surgery is considered if serum calcium is 1 mg/dL above normal, bone density T-score is below -2.5, creatinine clearance is under 60 mL/min, or the patient is under 50 years old. For secondary hyperparathyroidism, surgery is considered if PTH exceeds 800 ng/L, does not respond to treatment, or in cases of renal osteodystrophy or calciphylaxis.
Does vitamin D deficiency increase parathyroid hormone?
Yes, vitamin D deficiency increases parathyroid hormone (PTH). Without adequate vitamin D, intestinal calcium absorption decreases, lowering blood calcium, prompting the parathyroid glands to secrete more PTH—this is secondary hyperparathyroidism. The increase in PTH aims to raise calcium by increasing bone resorption.
What are the symptoms of high parathyroid hormone?
Symptoms include bone pain or tenderness, depression, forgetfulness, fatigue, kidney stones, frequent urination, nausea, and loss of appetite. Muscle weakness, constipation, abdominal pain, and concentration problems are also common. These result from the effects of excess PTH on calcium metabolism and may cause hypercalcemia.
Why is parathyroid hormone high?
High PTH usually results from one or more parathyroid glands being overactive, commonly due to a benign tumor or gland enlargement. Secondary hyperparathyroidism occurs with chronic kidney disease or vitamin D deficiency. Tertiary hyperparathyroidism arises when the glands remain overactive even after the original problem is corrected.
What functions does PTH regulate in the body?
Parathyroid hormone (PTH) regulates calcium and phosphate balance. It increases bone resorption to raise calcium, supports kidney calcium reabsorption, activates vitamin D for increased intestinal absorption, and promotes phosphate excretion.
Which diseases are associated with high PTH?
High PTH is primarily seen in primary, secondary, and tertiary hyperparathyroidism. Primary hyperparathyroidism is usually due to a benign adenoma and is more frequent in women. Secondary hyperparathyroidism is linked to vitamin D deficiency or chronic kidney disease. Tertiary occurs after long-standing secondary hyperparathyroidism. High PTH is also associated with increased cardiovascular mortality.
How does low parathyroid hormone affect calcium balance?
Low PTH (hypoparathyroidism) decreases kidney calcium reabsorption and bone release, resulting in hypocalcemia. Most cases develop after neck surgery. Regular calcium and vitamin D supplementation is required, and ongoing monitoring of serum levels is crucial. Hypoparathyroidism may also lead to hyperphosphatemia.
How are high or low PTH levels treated?
High PTH (hyperparathyroidism) is usually treated by removing the overactive gland. If surgery is not an option, medications such as bisphosphonates and calcimimetics are prescribed. Low PTH (hypoparathyroidism) is treated with oral calcium and active vitamin D, and in resistant cases, PTH replacement may be considered. Regular monitoring and personalized plans are necessary.
What tests are performed to regulate PTH levels?
Tests include blood tests (calcium, PTH, phosphorus, creatinine, vitamin D), urine tests (24-hour urine calcium and creatinine), bone mineral density scans (DEXA), and imaging (ultrasound, CT, MRI, sestamibi scans) to localize overactive glands before surgery and monitor treatment.

Girişimsel Radyoloji ve Nöroradyoloji Uzmanı Prof. Dr. Özgür Kılıçkesmez, 1997 yılında Cerrahpaşa Tıp Fakültesi’nden mezun oldu. Uzmanlık eğitimini İstanbul Eğitim ve Araştırma Hastanesi’nde tamamladı. Londra’da girişimsel radyoloji ve onkoloji alanında eğitim aldı. İstanbul Çam ve Sakura Şehir Hastanesi’nde girişimsel radyoloji bölümünü kurdu ve 2020 yılında profesör oldu. Çok sayıda uluslararası ödül ve sertifikaya sahip olan Kılıçkesmez’in 150’den fazla bilimsel yayını bulunmakta ve 1500’den fazla atıf almıştır. Halen Medicana Ataköy Hastanesi’nde görev yapmaktadır.







Vaka Örnekleri