Pelvic congestion syndrome (PCS) is a chronic condition caused by dilated pelvic veins. It leads to persistent pelvic pain, particularly in women of reproductive age, and often worsens after prolonged standing or during menstruation.
Symptoms include pelvic heaviness, lower back pain, painful intercourse, and visible varicose veins in the genital or thigh area. These complaints often persist for months, significantly reducing quality of life.
Diagnosis relies on ultrasound, CT, or MR venography to detect abnormal pelvic veins. Interventional venography provides both confirmation and treatment planning for effective symptom management.
Endovascular embolization is the most effective treatment for PCS. By closing dilated veins, it relieves pain, restores venous circulation, and offers a minimally invasive alternative to surgical procedures.
| Disease Name | Pelvic Congestion Syndrome (PCS) |
| Definition | A chronic pain syndrome caused by dilation and pooling of blood in the veins (venous vessels) in the pelvic region. It is usually seen in women. |
| Symptoms | Chronic pelvic pain (usually lasting more than 6 months), a feeling of pressure in the groin or lower back, pain during or after intercourse, increased pain during menstruation, a feeling of fullness in the lower abdomen, and changes in urinary and bowel habits. |
| Causes | Backward flow of blood due to insufficiency of valves in the pelvic veins leads to venous dilation and pooling of blood. Vein dilation during pregnancy and hormonal changes can also be causes. |
| Risk Factors | Having had multiple pregnancies, high estrogen levels, a history of pelvic varices, prolonged standing or sitting, family predisposition. |
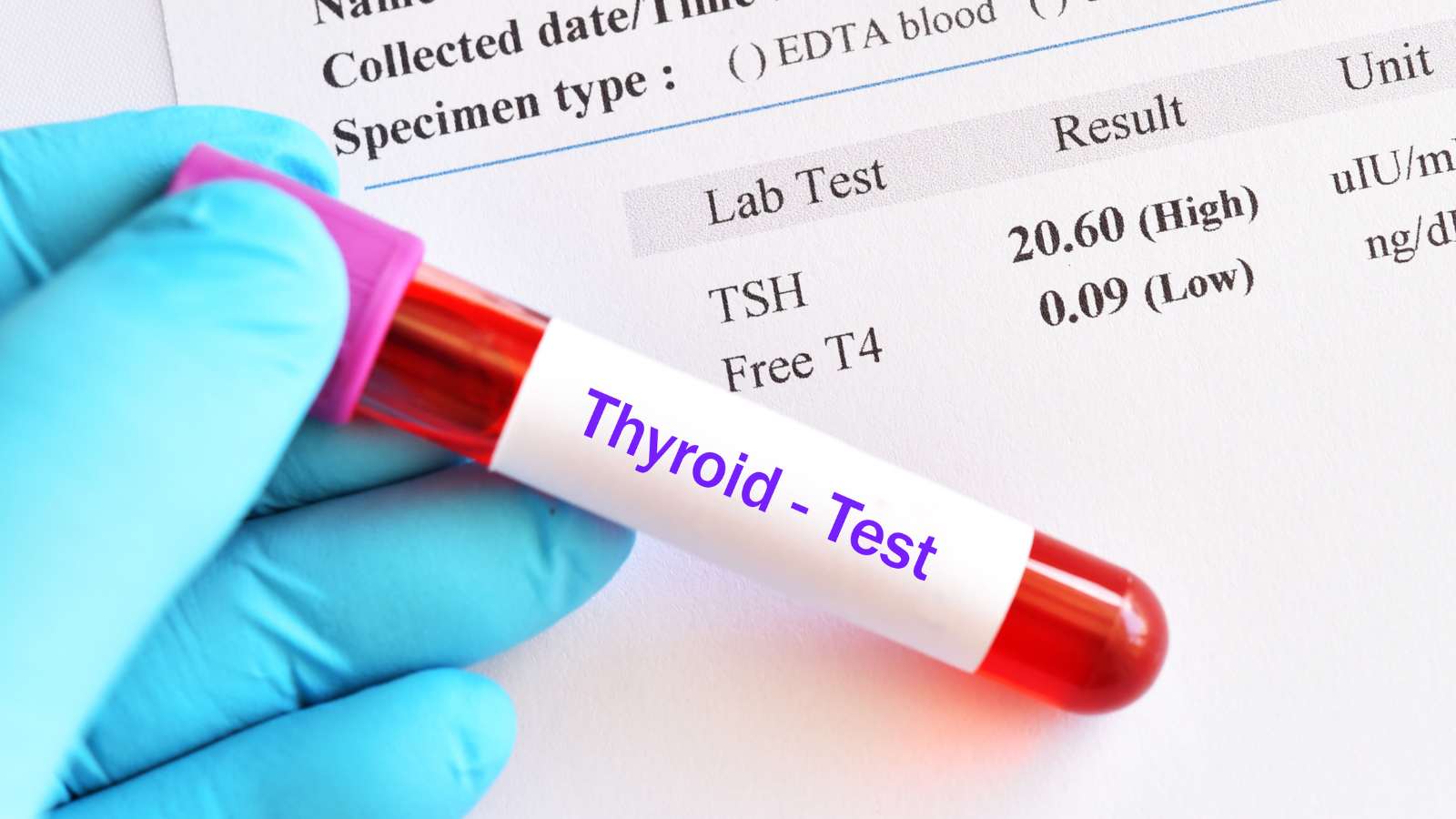
| Diagnostic Methods | Pelvic ultrasound, Doppler ultrasound, magnetic resonance imaging (MRI), computed tomography (CT), venography (for detailed visualization of the veins). |
| Treatment Methods | Pain medications, hormonal therapy (to reduce vein dilation), minimally invasive procedures (pelvic vein embolization), and rarely, surgical intervention. |
| Complications | Chronic pain due to pooling of blood in the pelvic organs, sexual dysfunction, decreased quality of life, and rarely, formation of blood clots (thrombosis). |
| Surgical Requirement | Surgical treatment may be considered in severe cases unresponsive to other therapies; procedures such as ligation or removal of veins may be performed. |
| Recovery Time | Varies depending on the treatment; patients usually recover within a few days after embolization, while a few weeks may be needed after surgery. |
| Prevention Methods | Avoiding prolonged standing or sitting, regular exercise, healthy weight control, and regular pelvic examinations during pregnancy. |
Prof. Dr. Özgür KILIÇKESMEZ Prof. Dr. Kılıçkesmez holds the Turkish Radiology Competency Certificate, the Turkish Interventional Radiology Competency Certificate, Stroke Treatment Certification, and the European Board of Interventional Radiology (EBIR). In his academic career, he won the Siemens Radiology First Prize in 2008.
Interventional Radiology / Interventional Neuroradiology
What is Pelvic Congestion Syndrome?
Pelvic Congestion Syndrome (PCS) is a chronic condition that causes prolonged pain in the pelvic area. In this syndrome, enlarged veins and malfunctioning valves lead to backward blood flow. This backward flow causes pooling and increased pressure in the vein walls, resulting in pain. Especially, the dilation of veins and accumulation of blood increases discomfort by pressing on nerves. PCS is mostly associated with changes in the veins during pregnancy and high estrogen levels. Although it is generally seen in premenopausal women, it can affect different age groups as well. As a result, PCS can significantly affect women’s quality of life.
What Are the Causes of Pelvic Congestion Syndrome?
The causes of Pelvic Congestion Syndrome (PCS) arise from a combination of several main factors. Firstly, venous insufficiency and reflux are among the primary reasons. Malfunctions in the valves of the pelvic region cause backward blood flow, leading to pelvic congestion. In addition, increased estrogen levels during pregnancy and hormonal changes in the menstrual cycle are among the triggering factors for PCS.
The effects of hormonal changes on pelvic veins are quite significant. An increase in estrogen leads to vein dilation and predisposes to varicose veins.
In addition, having multiple births also plays a role in the development of PCS in some women. The increased blood volume and physical changes during pregnancy can lead to pelvic vein dilation and venous dysfunction. Additionally, certain anatomical variations may increase the risk of PCS.
- Nutcracker Syndrome: This condition, resulting from the compression of the left renal vein, can cause backward blood flow in the pelvic veins.
- May-Thurner Syndrome: This syndrome, caused by the compression of the left iliac vein, can lead to venous hypertension and increase the risk of PCS.
Finally, genetic predisposition and lifestyle factors should not be overlooked. Genetic tendencies related to vein wall weakness can trigger PCS. Lifestyle factors such as obesity also contribute to increased venous pressure and may worsen symptoms. These elements play an important role in the onset and progression of PCS.
*We recommend filling out all fields so we can respond in the best possible way.
How Common Is Pelvic Congestion Syndrome?
The prevalence of Pelvic Congestion Syndrome (PCS) varies according to studies but is particularly high among women suffering from chronic pelvic pain. Research shows that this condition can be seen in 10% to 40% of women. In addition, it is noted that up to 60% of women with ovarian vein enlargement are at risk of developing PCS.
PCS generally affects premenopausal women and is more common in those who have had multiple pregnancies. The average age at diagnosis is between 30 and 50. PCS is observed not only in women of reproductive age but also in postmenopausal women. This indicates that the prevalence of PCS may be higher than traditionally thought.
PCS symptoms include chronic pelvic pain, dysmenorrhea, and dyspareunia, and are also associated with the following situations:
- Increased pain during prolonged standing or sitting
- Varicose veins in the vulva and lower extremities
- Psychological stress resulting from pelvic discomfort
Psychologically, PCS may lead to problems such as depression in 25% to 50% of patients. Population-based studies using imaging techniques have detected pelvic varices in 38% to 47% of asymptomatic women. This suggests that the potential prevalence of PCS may be higher than reported. As a result, more comprehensive research is needed to understand the true prevalence of PCS.
How Does Pelvic Congestion Syndrome Develop?
Pelvic Congestion Syndrome (PCS) is a chronic condition that develops due to dysfunction of the pelvic veins. Venous valve insufficiency, hormonal effects, and the complexity of pelvic anatomy play roles in the development of PCS. Firstly, venous valve insufficiency forms the main mechanism of the syndrome. Normally, these valves prevent the backward flow of blood, but when they fail, blood flows backward and vein pressure increases.
Over time, dysfunction of these valves leads to the development of varices. Enlarged pelvic veins become tortuous, increasing blood pooling and causing chronic pain. Hormonal effects also play a decisive role in the development of PCS. Especially estrogen during pregnancy causes dilation of pelvic veins and worsens valve insufficiency, making women more susceptible to PCS.
The anatomical arrangement of pelvic veins also contributes to the onset of the syndrome. The venous system in this region forms a complex network, and in some cases, vascular obstruction further increases the effects of pelvic varices. Conditions such as May-Thurner and Nutcracker syndromes particularly contribute to secondary venous obstruction.
What Are the Symptoms of Pelvic Congestion Syndrome?
Pelvic Congestion Syndrome (PCS) is a condition mainly characterized by chronic pelvic pain and decreased quality of life. This pain can last longer than six months and is often described as a dull, aching sensation. The pain becomes more pronounced during prolonged standing or sitting, as these positions increase pressure on the pelvic veins. Additionally, pain may increase during menstruation due to hormonal changes.
Symptoms of PCS include:
- Prolonged Standing or Sitting: Pain increases due to pressure on the pelvic veins.
- Menstrual Cycle: Hormonal changes increase vein dilation, worsening pain.
- Sexual Activity: Pain during or after intercourse is common and may result from swollen pelvic veins.
- Physical Exertion: Activities such as walking or heavy lifting further strain the enlarged veins, worsening symptoms.
- Pregnancy: Especially in subsequent pregnancies, increased hormones and intra-abdominal pressure may intensify symptoms.
In addition to chronic pelvic pain, other symptoms may also be observed. Complaints such as varicose veins in the thigh, hip, or vaginal area, and lower back pain that may radiate to the legs, can occur. Additionally, increased urinary frequency due to bladder pressure may be seen. Abdominal bloating and a feeling of heaviness in the pelvic area are also common symptoms. Since these symptoms may overlap with other pelvic disorders, diagnosis is often difficult and may require detailed imaging.
How Is Pelvic Congestion Syndrome Diagnosed?
The diagnosis of Pelvic Congestion Syndrome (PCS) requires the combination of various methods due to its complex nature and the similarity of its symptoms to other pelvic disorders. PCS usually presents with chronic pelvic pain lasting more than six months in premenopausal women. Clinical assessment and imaging techniques are used together to reach the correct diagnosis.
- Clinical Assessment: If a patient history reveals dull pelvic pain that worsens with standing, menstrual cycle, or sexual activity, PCS may be suspected. However, such symptoms can also be seen in many different diseases.
- Ultrasound: Transvaginal or transabdominal ultrasound can assess pelvic vein dilation. The status of the ovarian veins is specifically examined, but the sensitivity of this method may not always be high.
- Magnetic Resonance Imaging (MRI): MRI with contrast is an effective method for detecting dilated veins and excluding other causes of PCS. It is frequently preferred to rule out other causes of pain.
- CT Venography: Venography by computed tomography provides a detailed image of the pelvic venous system. This method can confirm dilation or reflux in the ovarian veins.
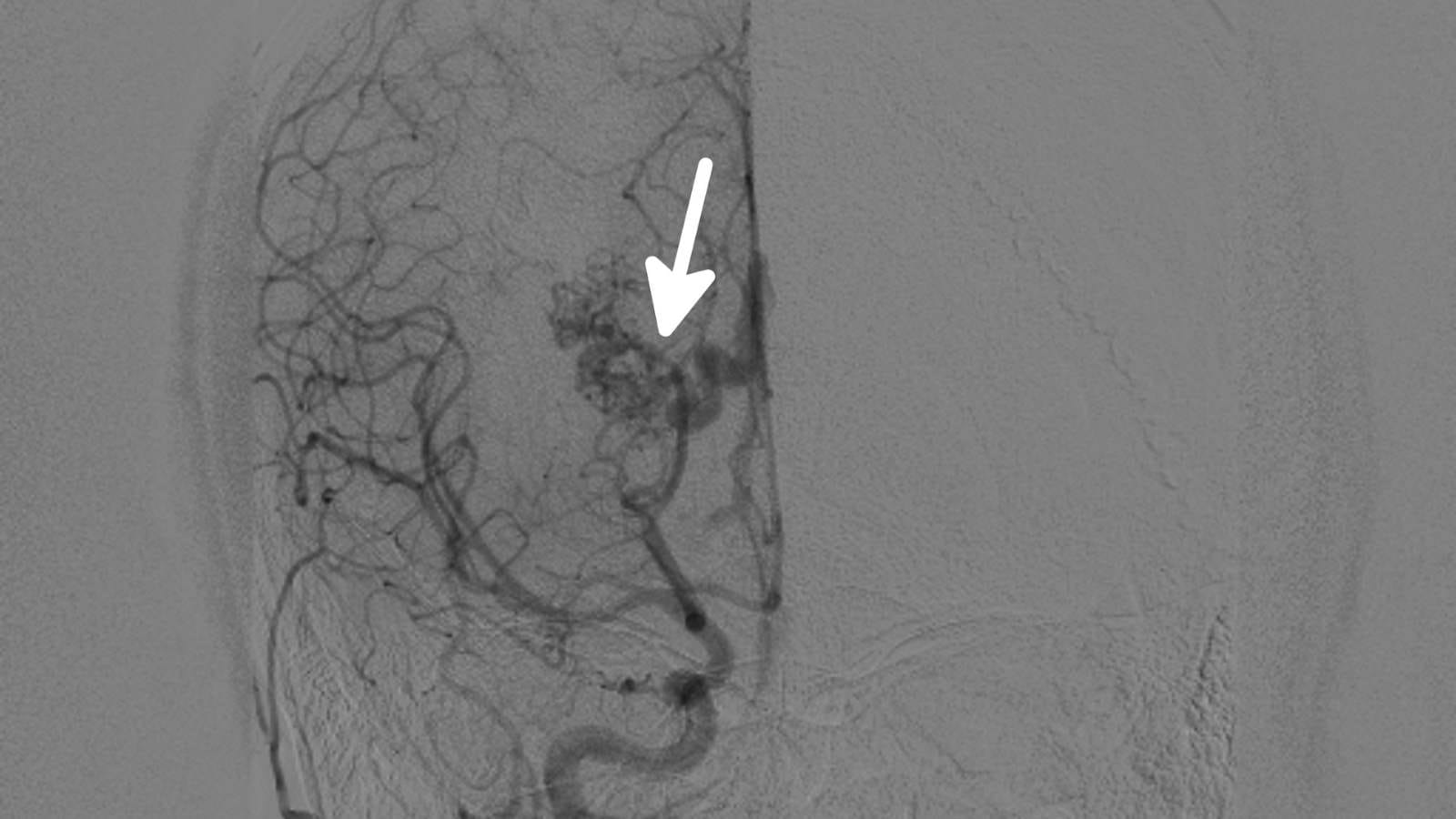
- Pelvic Venography: By injecting contrast into the pelvic veins, venography provides detailed images of the venous system. This is considered the gold standard, especially when other imaging methods are inadequate.
- Laparoscopy: Sometimes laparoscopy is performed to rule out other causes of pelvic pain, but due to advances in imaging techniques, it is now a less commonly used method.
How Is Pelvic Congestion Syndrome Treated?
Pelvic Congestion Syndrome (PCS) is usually treated with minimally invasive procedures, and pelvic vein embolization (PVE) is the main method. This procedure targets the enlarged veins causing chronic pelvic pain to relieve symptoms. Especially, interventions aimed at the enlarged ovarian and internal iliac veins contribute significantly to pain reduction. During embolization, various embolic materials are used to block the enlarged veins. These materials are placed into the vein under fluoroscopic guidance and block blood flow, providing relief.
Research on the effectiveness of PVE in PCS treatment shows marked improvement in most patients. Success rates vary depending on the type of material used and the specific characteristics of the treated veins.
- Embolization of only the ovarian veins: Provides improvement in more than 90% of patients.
- Combined treatment of both ovarian and internal iliac veins: Offers relief in up to 96% of cases.
PVE is considered a safe method and has a low complication rate. Most patients experience mild, temporary pain after the procedure, but permanent side effects are rare. Most often, patients can return to daily activities within 24 hours. Studies indicate that this method has high technical success rates, with 70-95% of patients experiencing significant relief from pelvic pain. Long-term follow-up results show a low recurrence of symptoms, but repeated procedures may be required in some cases.
What Are the Risk Factors for Pelvic Congestion Syndrome?
The risk factors for Pelvic Congestion Syndrome include many important factors that can lead to this condition in women. This syndrome, which mainly affects women of reproductive age, may develop due to various biological and lifestyle factors. Firstly, a history of pregnancy increases the risk of PCS. During pregnancy, the veins in the pelvis dilate and may not return to normal after birth, leading to venous insufficiency. Hormonal effects are also among the risk factors. Estrogen, especially during reproductive years, contributes to vein dilation and increases the likelihood of developing PCS.
Additionally, individuals with a family history of varicose veins or those with varicose veins in the legs are at risk for PCS. This may indicate underlying pelvic venous insufficiency. Pelvic venous insufficiency should be considered among the risk factors. Weak vein valves cause backward blood flow and vein dilation.
Furthermore, Nutcracker Syndrome and May-Thurner Syndrome are among the vascular compression syndromes that can affect PCS development. These conditions obstruct blood flow in the pelvic region.
When Can Pelvic Congestion Syndrome Be Treated?
The treatment of Pelvic Congestion Syndrome (PCS) is evaluated according to various criteria and usually requires interventional radiology procedures. One of the most important indications for treatment is chronic pelvic pain lasting more than six months and not attributable to another cause. This pain is often exacerbated by prolonged standing, sitting, sexual activity, or menstruation. Other conditions requiring treatment include pelvic vein dilation and signs of venous insufficiency. Especially, pelvic vein dilatation and reflux confirmed by imaging studies are important diagnostic indicators that guide treatment.
In addition, pelvic vein embolization should be considered in the following cases:
- Chronic pelvic pain: This long-lasting, non-cyclic pain increases with physical activity or prolonged standing.
- Venous insufficiency and varices: The presence of venous reflux and dilation in the ovarian or internal iliac veins detected by imaging methods such as MRI, Doppler ultrasound, or venography is important.
- Failed conservative therapy: In patients who do not achieve sufficient improvement with conservative methods such as hormonal therapy, pain management, or physical therapy, interventional procedures can be considered.
- Concurrent symptoms and pelvic varices: If there are prominent varicose veins in the vulvar, perineal, or thigh regions, treatment is necessary.
- Associated venous syndromes: Conditions such as Nutcracker or May-Thurner syndrome contribute to venous hypertension in PCS and should be included in the treatment plan.
- Multiple pregnancies: Repeated pregnancies can intensify PCS symptoms with increased vein dilation.
When Can Pelvic Congestion Syndrome Not Be Treated?
Interventional radiology procedures used in the treatment of Pelvic Congestion Syndrome (PCS), particularly transcatheter embolization, cannot be performed in certain situations. Various contraindications include situations where this treatment may pose a risk or complicate the treatment process. The main situations in which embolization cannot be performed are as follows:
- Pregnancy: This procedure is not recommended during pregnancy due to the risk of harm to the fetus. Therefore, embolization therapy is generally not performed during pregnancy.
- Severe Allergy to Contrast Agents: Contrast agents are used during the procedure for better visualization of the veins. However, patients with severe allergic reactions to these agents are not considered suitable candidates for embolization.
- Coagulopathy or Uncontrolled Bleeding Disorders: Embolization may be risky in individuals with bleeding disorders or those receiving anticoagulant therapy. Uncontrolled bleeding can cause complications during or after the procedure.
- Renal Failure: The contrast agents used during embolization can damage the kidneys. This carries a greater risk in individuals with impaired renal function, and treatment is not recommended.
- Pelvic Malignancy: Alternative treatment options are considered in the presence of malignancy in the pelvic area. Malignancy can adversely affect the success of embolization therapy.
- Severe Pelvic Infections: Embolization is not recommended in patients with active pelvic infections. These situations are considered contraindications due to the risk of systemic spread and worsening of the infection.
- Pelvic Thrombosis: Embolization should not be performed in individuals with pelvic thrombosis. This increases the risk of clot migration during the procedure and reaching the lungs.
What Is the Recovery Process After Pelvic Congestion Syndrome Treatment?
The recovery process after embolization treatment for Pelvic Congestion Syndrome (PCS) is usually quick and uneventful. Many patients are discharged on the same day after this minimally invasive procedure and do not require prolonged hospitalization. Mild cramps and lower abdominal pain may occur during the first week but these symptoms generally resolve quickly.
- Pain can be easily managed with over-the-counter medications.
- Mild side effects such as slight fever and fatigue in some patients resolve within a few days.
- Patients can generally return to daily activities 3–7 days later.
However, avoiding strenuous physical activity is recommended after treatment. In the long term, most patients experience significant symptom relief and a substantial reduction in chronic pain. However, it is known that symptoms may rarely recur after treatment.
How Can Pelvic Congestion Syndrome Be Prevented?
Reducing risk factors and supporting venous circulation are important for the prevention of Pelvic Congestion Syndrome (PCS). Regular exercise reduces pooling of blood in the pelvic region and increases venous return. Similarly, maintaining a healthy weight can reduce pressure on the pelvic veins. Avoiding prolonged sitting or standing is also effective in preventing blood stagnation. Additionally, controlling hormonal levels may reduce vein dilation.
Recommended preventive strategies include:
- Regular Exercise: Improves blood circulation in the pelvic area.
- Healthy Weight Management: Supports venous health by reducing additional pressure.
- Changing Position: Avoid staying in the same position for long periods.
- Hormonal Management: Controlling estrogen levels may be beneficial.
- Pregnancy Planning: Preventing frequent pregnancies can help protect vein health.

Girişimsel Radyoloji ve Nöroradyoloji Uzmanı Prof. Dr. Özgür Kılıçkesmez, 1997 yılında Cerrahpaşa Tıp Fakültesi’nden mezun oldu. Uzmanlık eğitimini İstanbul Eğitim ve Araştırma Hastanesi’nde tamamladı. Londra’da girişimsel radyoloji ve onkoloji alanında eğitim aldı. İstanbul Çam ve Sakura Şehir Hastanesi’nde girişimsel radyoloji bölümünü kurdu ve 2020 yılında profesör oldu. Çok sayıda uluslararası ödül ve sertifikaya sahip olan Kılıçkesmez’in 150’den fazla bilimsel yayını bulunmakta ve 1500’den fazla atıf almıştır. Halen Medicana Ataköy Hastanesi’nde görev yapmaktadır.






Vaka Örnekleri