A hemangioma is a benign vascular tumor often appearing as a birthmark during infancy. It results from an abnormal proliferation of blood vessels and can occur on the skin, subcutaneous tissue, or internal organs. Most cases are harmless and regress spontaneously.
Infantile hemangiomas typically appear within the first weeks of life and may grow rapidly before gradually shrinking. While most resolve without treatment, medical intervention may be needed if the lesion affects vision, breathing, or feeding.
Hemangioma treatment options include observation, beta-blocker therapy, laser treatment, or minimally invasive procedures. The method depends on the lesion’s size, location, and impact on organ function.
Vascular birthmark management requires careful follow-up by specialists. Early diagnosis helps determine which hemangiomas need intervention and ensures timely treatment to prevent functional or cosmetic complications.
What Is a Hemangioma and How Does It Develop?
A hemangioma is a benign tumor and is non-cancerous. It is mostly seen in infants and begins to appear within the first weeks of life. It usually manifests as a red or purple birthmark on the skin, but it can also occur in internal organs such as the liver. This health issue can be observed in various parts of the body. The most common locations are:
- Face
- Scalp
- Chest
- Back
- Arms and legs
It occurs due to the pooling of blood in small lakes within abnormal blood vessels. This abnormal growth of blood vessels usually results from improper formation of vessels during pregnancy. In adults, it can sometimes develop after an injury or following various illnesses. However, the exact causes of these situations are not fully known. Each hemangioma case may differ and growth rates may vary. Research on hemangioma development is ongoing.
What Are the Symptoms of Hemangioma?
Hemangioma symptoms vary depending on the type and location.
Appearance:
- Superficial hemangiomas appear as bright red, raised, bumpy lesions on the skin; these are often described as “strawberry marks.”
- Deep hemangiomas have a bluish and swollen appearance beneath the skin.
- Mixed hemangiomas combine both superficial and deep features.
Regarding growth and development, hemangiomas usually become apparent within the first weeks after birth. They grow rapidly in the first few months and this growth begins to slow around 5–8 months. Most hemangiomas start to shrink naturally when the child is between 5 and 10 years old. This process may vary depending on the type and size of the hemangioma. Especially large or strategically located hemangiomas may cause appearance and functional problems.
What Are the Types of Hemangioma?
Hemangioma types vary depending on their location and characteristics. Superficial hemangiomas appear as bright red marks like strawberry spots on the skin. Deep hemangiomas form in the deeper layers of the skin and may take on a bluish-purple color. Mixed hemangiomas, formed by the combination of these two types, can affect both the upper and deeper tissues of the skin. Infantile hemangiomas are the most common type in children, typically appearing soon after birth and begin to shrink within a few years. Congenital hemangiomas are present at birth and may be of types that regress rapidly or do not shrink at all. Cavernous hemangiomas occur in adults as small groups of red spots on the trunk. Intramuscular hemangiomas develop within muscle tissue and can cause pain that increases with activity. Bone hemangiomas are often asymptomatic and are usually found in the skull and spine. Internal organ hemangiomas are located in organs such as the liver and intestines and are generally asymptomatic. Segmental hemangiomas are large and can spread over a wide area of the body, carrying a high risk of complications. This diversity is an important factor in the diagnosis and treatment of hemangiomas.
Who Is More Likely to Have Hemangiomas?
Hemangiomas tend to be more common in certain groups. This condition is frequently seen in infants. About five percent of newborns are affected, and the rate is three times higher in girls than in boys. Additionally, premature birth and low birth weight increase the risk of hemangioma development.
- Newborn infants
- Female infants
- Premature infants
- Low birth weight infants
- Fair-skinned infants
In adults, the situation is different. Hemangiomas generally start to appear after the age of 30. In women, especially those receiving hormone replacement therapy or during pregnancy, liver hemangiomas are more common than in men. This is due to the effect of estrogen.
- Adults over 30
- Especially women
- Those on hormone replacement therapy
- Pregnant women
Hemangiomas are also common in older adults. More than half of people over the age of 60 have at least one hemangioma. These hemangiomas are usually small and often located in internal organs.
These groups are at higher risk of developing hemangiomas. In all cases, doctors determine the most appropriate treatment methods based on the characteristics of the patients.
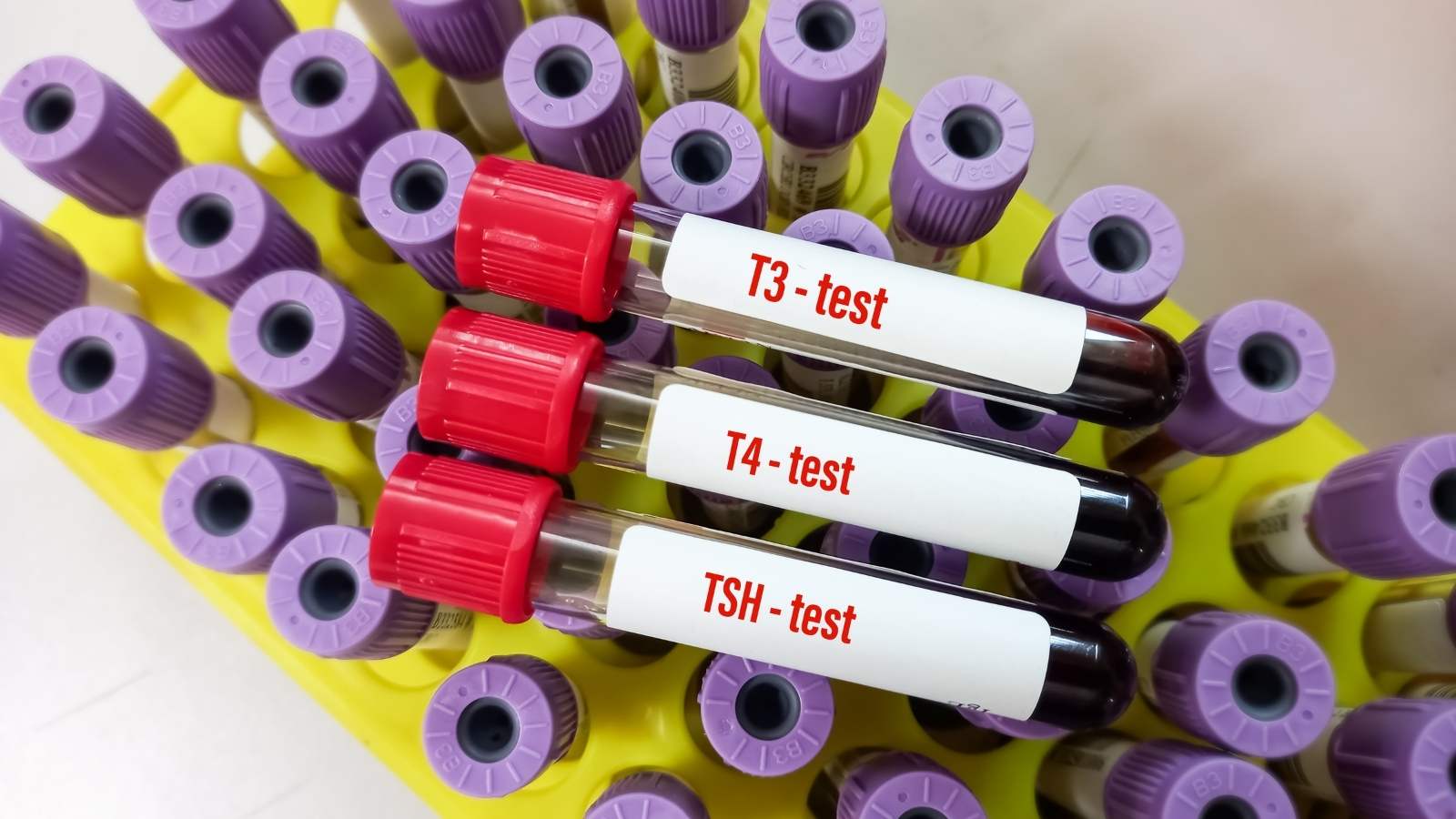
How Is Hemangioma Diagnosed?
Hemangiomas are usually diagnosed by visual examination and special imaging tests. Superficial hemangiomas are easily noticed during a doctor’s physical examination. Doctors can often identify these hemangiomas just by their appearance. For deeper or internal organ hemangiomas, more detailed examinations are required. In such cases, various imaging methods are used to support the diagnosis and rule out other health problems:
Ultrasound:
Used to determine the location and size of subcutaneous hemangiomas.
Computed Tomography (CT) Scans:
Evaluates the effect of the hemangioma on surrounding tissues.
Magnetic Resonance Imaging (MRI):
Provides detailed images of both superficial and deep tissue hemangiomas.
Although most hemangiomas are diagnosed by observation, in suspicious or complex cases, a biopsy can be performed for definitive diagnosis.
What Are the Treatment Methods for Hemangioma?
Hemangioma treatment varies depending on the location, size, and symptoms of the lesion. Various interventional methods are used in the management of hemangioma. One of these methods is Transarterial Embolization. Embolic agents are injected into the arteries feeding the hemangioma to shrink the tumor. This method is especially preferred for symptomatic hepatic hemangiomas. Transarterial Chemoembolization is also an effective option for more aggressive hemangiomas, combining embolization with chemotherapy.
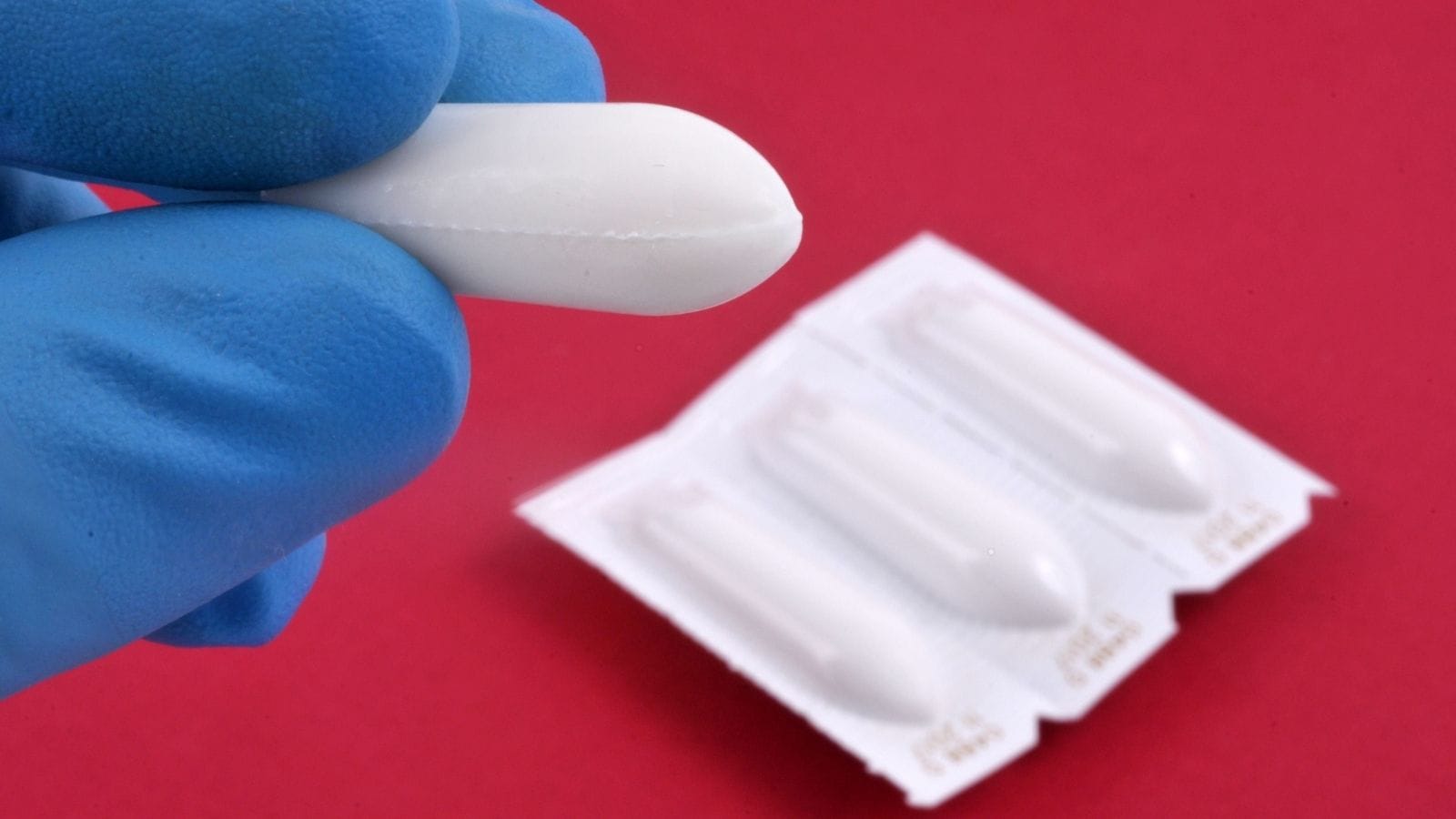
Sclerotherapy:
A very simple, short procedure with almost no risk, similar to varicose veins. Polidocanol mixed with air is injected into the lesion with a small needle. The lesion does not disappear but shrinks; most importantly, the patient’s complaints are almost completely resolved. However, depending on the size of the lesion, many sessions may be needed.
Propranolol Therapy:
Propranolol, a beta blocker, is especially preferred for treating infantile hemangiomas.
Radiofrequency Ablation:
This minimally invasive technique destroys tumor cells using radiofrequency energy and is suitable for cases not amenable to surgery.
Surgical Resection is considered for hemangiomas with a high risk of complications or those that are rapidly growing.
What Are the Risk Factors for Hemangioma?
Various factors affect the risk of developing hemangioma. Girls are more often affected than boys. The incidence is higher among Caucasian infants. Premature birth and low birth weight are also risk factors. Family history increases the likelihood of this health issue. Hemangioma is also more common in mothers expecting multiple children. Pregnancy complications, especially placenta previa and preeclampsia, are other important risk factors. Advanced maternal age also contributes to this condition. As for liver hemangiomas:
Age:
Usually seen between the ages of 30 and 50.
Gender:
More frequently diagnosed in women.
Pregnancy:
Hormonal changes during this period may trigger hemangioma growth.
Hormone Replacement Therapy:
The use of this therapy can also increase the risk.
How to Distinguish Hemangioma from Other Skin Lesions?
Hemangiomas show distinct differences on the skin and can be differentiated from other vascular lesions. They are generally classified as either infantile or congenital. Both types have specific features and are diagnosed through clinical evaluation.
Appearance and Growth Pattern:
- Infantile hemangiomas appear as bright red, rubbery raised bumps or flat red patches.
- These lesions appear within the first weeks of life, grow rapidly in the first year, and generally regress slowly by the age of ten.
- Congenital hemangiomas are already fully formed at birth, and either shrink rapidly within the first year or remain the same size.
**Color and Texture:**
- They range in color from red to blue, most commonly in soft tissue.
- Superficial hemangiomas are bright red, while deeper ones may be bluish and spongy.
**Location and Symptoms:**
- They are most commonly seen on the face, scalp, chest, or back.
- They are usually painless but may cause complications if located in critical anatomical areas.
Compared to other vascular lesions, hemangiomas are notable for their phases of growth and regression. Some vascular lesions, such as arteriovenous malformations, have a stable or very slow growth rate. These lesions often require medical intervention due to their potential complications.
What Is the Healing Process of Hemangioma?
The healing process after hemangioma treatment varies depending on the type of treatment. After transarterial embolization, patients can generally return to normal life within the first week. Initial pain is managed with appropriate medications, and patients are monitored regularly.
Initial Recovery: Pain and mild fever after the procedure
Follow-up: Regular checkups and imaging
Long Term: Symptom reduction as the hemangioma shrinks
For cases requiring surgical intervention, patients may stay in the hospital for a few days post-surgery. Pain management and wound care are critical in this process.
Initial Recovery: Hospital stay after surgery
Follow-up: Regular visits for infection monitoring
Long Term: Complete healing and return to activities
Propranolol therapy is an alternative to surgery and usually shows effects within a few weeks. Initial monitoring is important for dose adjustments and management of side effects.
Initial Recovery: Effects within the first few weeks
Follow-up: Monitoring progress
Long Term: Gradual dose reduction and completion of treatment
Laser therapy often provides rapid healing with mild pain and redness at the treatment area. Multiple sessions may be required, and complete healing can take several weeks.
Initial Recovery: Redness and mild pain after treatment
Follow-up: Assessment of skin response
Long Term: Complete recovery of the area
Sclerotherapy involves injecting a sclerosing agent into the hemangioma, with initial recovery typically following the injection. Follow-up visits are needed to ensure proper healing and treatment efficacy. The treatment takes 5 minutes, the patient leaves walking, and can be repeated every 3–4 weeks.
Initial Recovery: Pain and swelling after injection
Follow-up: Sessions at intervals of a few weeks
Long Term: Shrinking of the hemangioma and clearer results

Girişimsel Radyoloji ve Nöroradyoloji Uzmanı Prof. Dr. Özgür Kılıçkesmez, 1997 yılında Cerrahpaşa Tıp Fakültesi’nden mezun oldu. Uzmanlık eğitimini İstanbul Eğitim ve Araştırma Hastanesi’nde tamamladı. Londra’da girişimsel radyoloji ve onkoloji alanında eğitim aldı. İstanbul Çam ve Sakura Şehir Hastanesi’nde girişimsel radyoloji bölümünü kurdu ve 2020 yılında profesör oldu. Çok sayıda uluslararası ödül ve sertifikaya sahip olan Kılıçkesmez’in 150’den fazla bilimsel yayını bulunmakta ve 1500’den fazla atıf almıştır. Halen Medicana Ataköy Hastanesi’nde görev yapmaktadır.







Vaka Örnekleri