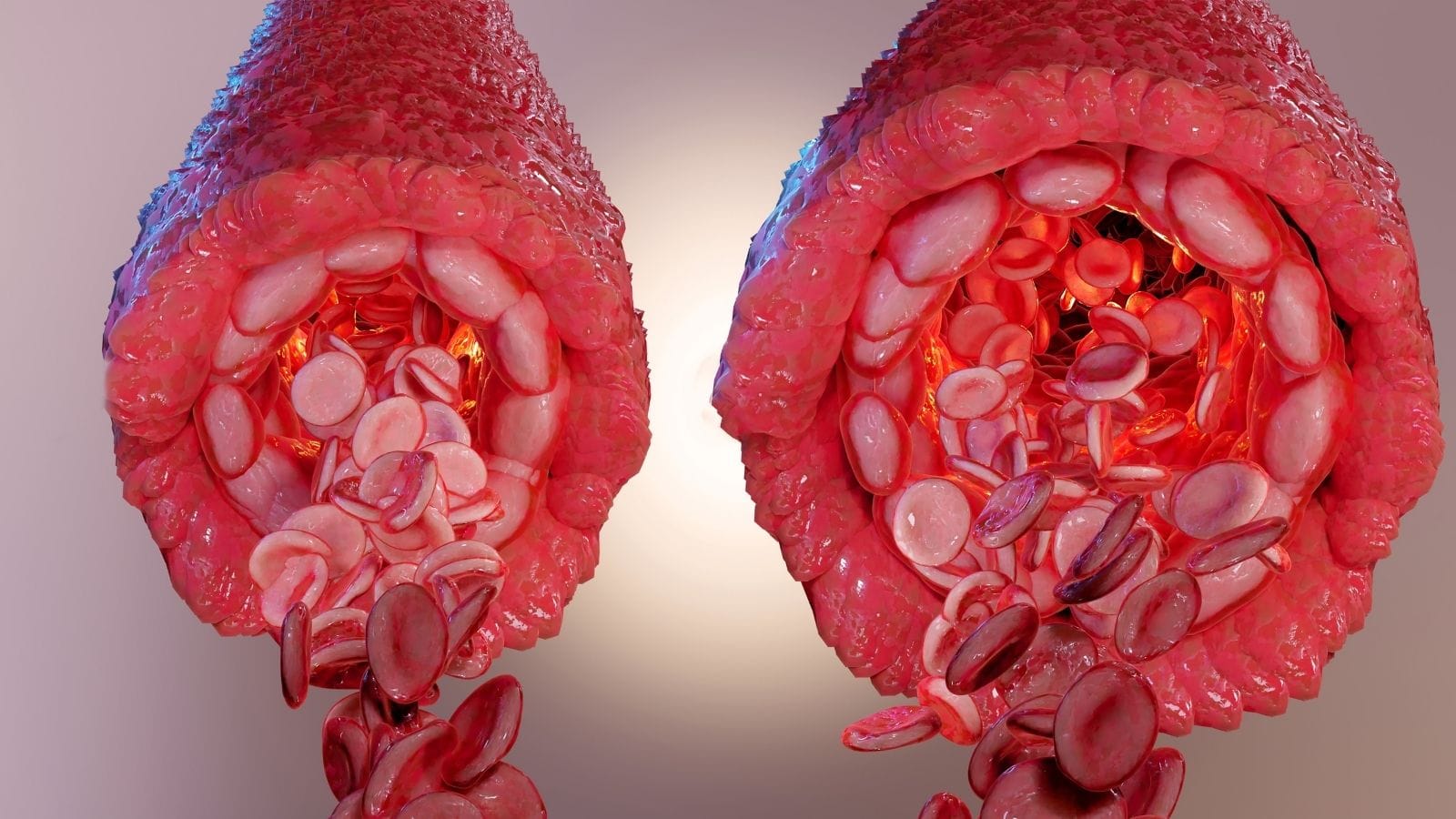
A dural arteriovenous fistula (DAVF) is an abnormal connection between a meningeal artery and a dural venous sinus or cortical vein. It causes altered blood flow patterns that may lead to neurological symptoms.
DAVF clinical signs include pulsatile tinnitus, headaches, vision problems, or neurological deficits. Severity depends on venous drainage patterns and the presence of cortical venous reflux.
Diagnosis of dural arteriovenous fistulas relies on digital subtraction angiography, which provides precise mapping of feeding arteries and draining veins. MRI and CT may also assist in initial evaluation.
DAVF treatment options include endovascular embolization, microsurgery, or radiosurgery. The choice depends on location, venous drainage, and risk of hemorrhage or neurological damage.
| Disease Name | Dural Arteriovenous Fistula (DAVF) |
| Definition | An abnormal connection (fistula) between arteries and veins in the brain’s outer membrane (dura mater), causing blood to flow abnormally between vessels. |
| Symptoms | Headache, pulsatile tinnitus (synchronous with the heartbeat), seizures, neurological deficits, double vision, signs of increased intracranial pressure, and rarely, brain hemorrhage. |
| Causes | Most often idiopathic, but may be associated with head trauma, infections, sinus thrombosis, surgical procedures, or hormonal changes. |
| Risk Factors | Middle and advanced age, history of head trauma, intracranial vascular disease, prior brain surgery, sinus thrombosis. |
| Diagnostic Methods | Brain MR or CT angiography, DSA (digital subtraction angiography – the most detailed method), MR venography, transcranial Doppler. |
| Treatment Methods | Endovascular embolization (injecting an embolic agent via catheter to close the fistula), surgical resection (removal of the fistula), radiosurgery (e.g., gamma knife). |
| Complications | Brain hemorrhage, seizures, nervous system damage, permanent neurological deficits, and if untreated, permanent brain injury and loss of function. |
| Follow-up and Monitoring | Regular imaging (MR or angiography) after treatment to monitor fistula closure and possible recurrence; ongoing neurological assessment. |
| Prevention Methods | No definitive prevention; avoiding head trauma and adopting vascular health-promoting lifestyle choices may reduce risk. |
| Treatment Response | Endovascular and surgical interventions usually yield successful outcomes; early diagnosis and treatment improve prognosis. |
Prof. Dr. Özgür KILIÇKESMEZ Prof. Dr. Kılıçkesmez holds the Turkish Radiology Competency Certificate, the Turkish Interventional Radiology Competency Certificate, Stroke Treatment Certification, and the European Board of Interventional Radiology (EBIR). In his academic career, he won the Siemens Radiology First Prize in 2008.
Interventional Radiology / Interventional Neuroradiology
What Is a Dural Arteriovenous Fistula (DAVF)?
A dural arteriovenous fistula (DAVF) is a rare vascular disorder characterized by an abnormal connection between arteries and veins in the dura mater—the outermost membrane of the brain and spinal cord. This shunt bypasses the normal capillary network and allows blood to flow directly from arteries into veins, potentially increasing venous pressure. Unlike arteriovenous malformations (AVMs), which occur within the brain tissue itself, DAVFs are located in the dura and affect meningeal vessels.
DAVFs are most common in adults between 50 and 70 and are generally acquired. They may be linked to factors such as venous sinus thrombosis, head trauma, or infections. Unlike congenital AVMs, DAVFs are more common in adults. When abnormal flow is especially directed to cortical veins, the risk of brain hemorrhage increases. Severity of symptoms depends on the anatomical location of the fistula and the pattern of venous drainage.
What Are the Causes of Dural Arteriovenous Fistula?
DAVFs are complex vascular anomalies that may arise from various triggers. Venous sinus thrombosis (CVST) is a key factor, as increased venous pressure can promote abnormal arteriovenous connections. Angiogenesis after thrombosis may lead to the formation of new vessels and accelerate DAVF development.
Traumatic brain injury is another frequent cause, as physical trauma can disrupt the natural structure of dural arteries and veins, leading to abnormal connections. Head injuries, in particular, create a favorable environment for fistula formation. Surgical procedures can also lead to DAVF, with manipulation around venous sinuses triggering neovascularization. Chronic infections or inflammation may damage vessel walls and support DAVF development.
What Are the Symptoms of Dural Arteriovenous Fistula?
DAVF symptoms vary depending on the location and venous drainage pattern, and can significantly affect quality of life or cause serious health problems. Key symptoms include:
- Pulsatile tinnitus: Rhythmic sounds heard in sync with the heartbeat.
- Headaches: Often due to increased intracranial pressure and can vary in intensity.
- Visual disturbances: Blurred or double vision, especially if near the cavernous sinus.
- Neurological deficits: Numbness, muscle weakness, balance problems, and in advanced cases, seizures.
- Cognitive and psychiatric symptoms: Long-term venous congestion may cause memory loss and related issues.
- Hemorrhage: High risk of brain hemorrhage in cases with cortical venous drainage, which can trigger sudden stroke-like emergencies.
*We recommend filling out all fields so we can respond in the best possible way.
How Is Dural Arteriovenous Fistula Diagnosed?
DAVF diagnosis uses several advanced imaging methods for detailed assessment. MRI is a first-line, non-invasive technique used to evaluate brain tissue damage and the anatomy of the fistula, often supplemented by MR angiography (MRA) to observe shunt flow.
Diagnostic methods include:
- Magnetic Resonance Angiography (MRA): A time-resolved method that analyzes arterial and venous phases, providing real-time flow images to assess DAVF drainage patterns.
- Computed Tomography Angiography (CTA): Uses contrast to provide high-resolution vascular images, especially important in emergencies for detecting intracranial hemorrhage and identifying arterial feeders.
- Digital Subtraction Angiography (DSA): The gold standard for DAVF diagnosis, involving contrast injection and detailed X-ray images to precisely locate the fistula and, in severe cases, detect cortical venous reflux (CVR).
What Are the Treatment Options for Dural Arteriovenous Fistula?
DAVF treatment options depend on the location, patient status, and risk of hemorrhage, and include endovascular embolization, stereotactic radiosurgery, and microsurgical resection. Treatment choice is usually determined by the type of venous drainage and symptom severity.
- Endovascular Embolization: The first-line treatment, offering a minimally invasive approach. This technique blocks the abnormal connection to stop pathological blood flow and reduce hemorrhage risk. Liquid embolic agents or coils are used, especially for high-risk DAVFs with cortical venous drainage.
- Stereotactic Radiosurgery: A non-invasive option for DAVFs in surgically difficult locations. Focused radiation is delivered to close the abnormal connection gradually. Radiosurgery is suited for small, low-risk DAVFs but may take months to show results.
- Microsurgical Resection: Used when other treatments are insufficient or unsuccessful. The abnormal vessels are surgically removed by craniotomy, especially in complex or hard-to-reach DAVFs, or when endovascular embolization cannot be completed.
What Is the Prognosis for Patients with Dural Arteriovenous Fistula?
Prognosis for DAVF patients varies greatly depending on fistula type and severity, as well as the timing of diagnosis and treatment. Early diagnosis and treatment (via endovascular embolization or surgery) generally lead to positive outcomes, preventing serious complications and greatly improving symptoms. Untreated DAVFs, especially those with cortical venous drainage, carry significant risks, including stroke, seizures, and high intracranial hemorrhage risk.
In such cases, hemorrhagic death rates can be high, making timely intervention critical for survival and quality of life. Lower-risk DAVFs (especially without cortical venous drainage) have a much lower risk of complications and may not require urgent intervention. Monitoring is often recommended for patients with mild or no symptoms, and regular imaging allows early detection of dangerous changes.
Frequently Asked Questions
How is a dural arteriovenous fistula diagnosed? DAVF is diagnosed through imaging methods. CT scans can show brain swelling or hemorrhage, while MRI provides detailed images of the fistula and small bleeds. The most reliable tool is catheter-based cerebral angiography (DSA), which clearly defines the number, location, and anatomy of the fistula and associated arteries.
How do the symptoms differ from other vascular diseases?
DAVF forms due to abnormal connections between arteries and veins in the dura mater. Symptoms include headaches, pulsatile tinnitus, visual changes, eye swelling, and severe cases with neurological deficits such as seizures or muscle weakness. These symptoms are usually due to increased venous pressure causing brain swelling or bleeding. Unlike congenital vascular diseases, DAVF is often acquired (after trauma, infection, or sinus thrombosis). Diagnosis is made with imaging, and treatment options include endovascular, surgical, or radiosurgical closure of abnormal connections.
How effective is embolization in DAVF treatment?
Embolization is the primary method for DAVF treatment, and its success rate depends on the technique and fistula features. Transarterial Onyx embolization achieves complete obliteration in 55–85.7% of cases, with a major complication rate of about 4.1%. Transvenous embolization has success rates of 77.8–100%. For spinal DAVFs, surgical treatment has higher initial occlusion rates than endovascular methods, but recurrence may be more frequent. In general, embolization is effective, but outcomes depend on technique and anatomy.
What are the consequences of untreated DAVF?
Untreated DAVFs can cause significant neurological complications such as cognitive impairment and increased risk of hemorrhage. About 50% of patients, especially those with cortical venous reflux, show impairment in at least one cognitive area. Untreated DAVF can lead to progressive dementia, seizures, and other neurological problems due to venous hypertension and resulting brain damage. Early and accurate diagnosis and treatment are crucial to protect brain health.
How does quality of life change after treatment?
DAVF treatment greatly improves quality of life for most patients. About 80% of treated patients experience significant clinical improvement, with better motor function and reduced urinary/bowel symptoms. Surgical interventions yield positive outcomes in 90.1% of cases, with a permanent complication rate of 4%. Endovascular embolization achieves complete closure in 93.2% of patients within 3–6 months, and 93% show improvement or stability in the modified Rankin Score. Recurrence rates within three years are 4.5–11%, underscoring the need for continued monitoring. Timely, appropriate DAVF treatment generally leads to major improvements in quality of life for most patients.

Girişimsel Radyoloji ve Nöroradyoloji Uzmanı Prof. Dr. Özgür Kılıçkesmez, 1997 yılında Cerrahpaşa Tıp Fakültesi’nden mezun oldu. Uzmanlık eğitimini İstanbul Eğitim ve Araştırma Hastanesi’nde tamamladı. Londra’da girişimsel radyoloji ve onkoloji alanında eğitim aldı. İstanbul Çam ve Sakura Şehir Hastanesi’nde girişimsel radyoloji bölümünü kurdu ve 2020 yılında profesör oldu. Çok sayıda uluslararası ödül ve sertifikaya sahip olan Kılıçkesmez’in 150’den fazla bilimsel yayını bulunmakta ve 1500’den fazla atıf almıştır. Halen Medicana Ataköy Hastanesi’nde görev yapmaktadır.







Vaka Örnekleri