A blood thinner is a medication that prevents blood clot formation or reduces the risk of clot enlargement. These drugs are essential in the prevention and treatment of cardiovascular and thromboembolic diseases.
There are two main categories: anticoagulants, such as warfarin and DOACs, and antiplatelet agents, such as aspirin and clopidogrel. Each acts on different mechanisms in the clotting process.
Blood thinners are commonly prescribed for atrial fibrillation, deep vein thrombosis, pulmonary embolism, and after stent placement. They reduce the risk of stroke, heart attack, and systemic embolism.
Regular monitoring, dose adjustment, and awareness of bleeding risks are essential during treatment. Patient compliance ensures both safety and therapeutic effectiveness.
What Is a Blood Thinner?
Blood thinners are a group of drugs that intervene at specific stages of the blood clotting mechanism in our body. The clotting system is a complex process that prevents blood loss when bleeding occurs. You can think of it like a construction process: when there is damage in a blood vessel, the body quickly sends “repair team” clotting factors and platelets to the area. Using “bricks” (platelets) and “mortar” (fibrin network), this team builds a “temporary wall” to stop the bleeding.
However, sometimes this repair team works too much or at the wrong place and time, like adding an unnecessary wall on top of a solid one. This can lead to unwanted clots. Blood thinners prevent this excessive or misplaced construction, ensuring the healthy continuation of blood flow in the body.
When Are Blood Thinners Used?
Blood thinners are prescribed in various cardiovascular conditions and situations with a high risk of clot formation. Main uses include:
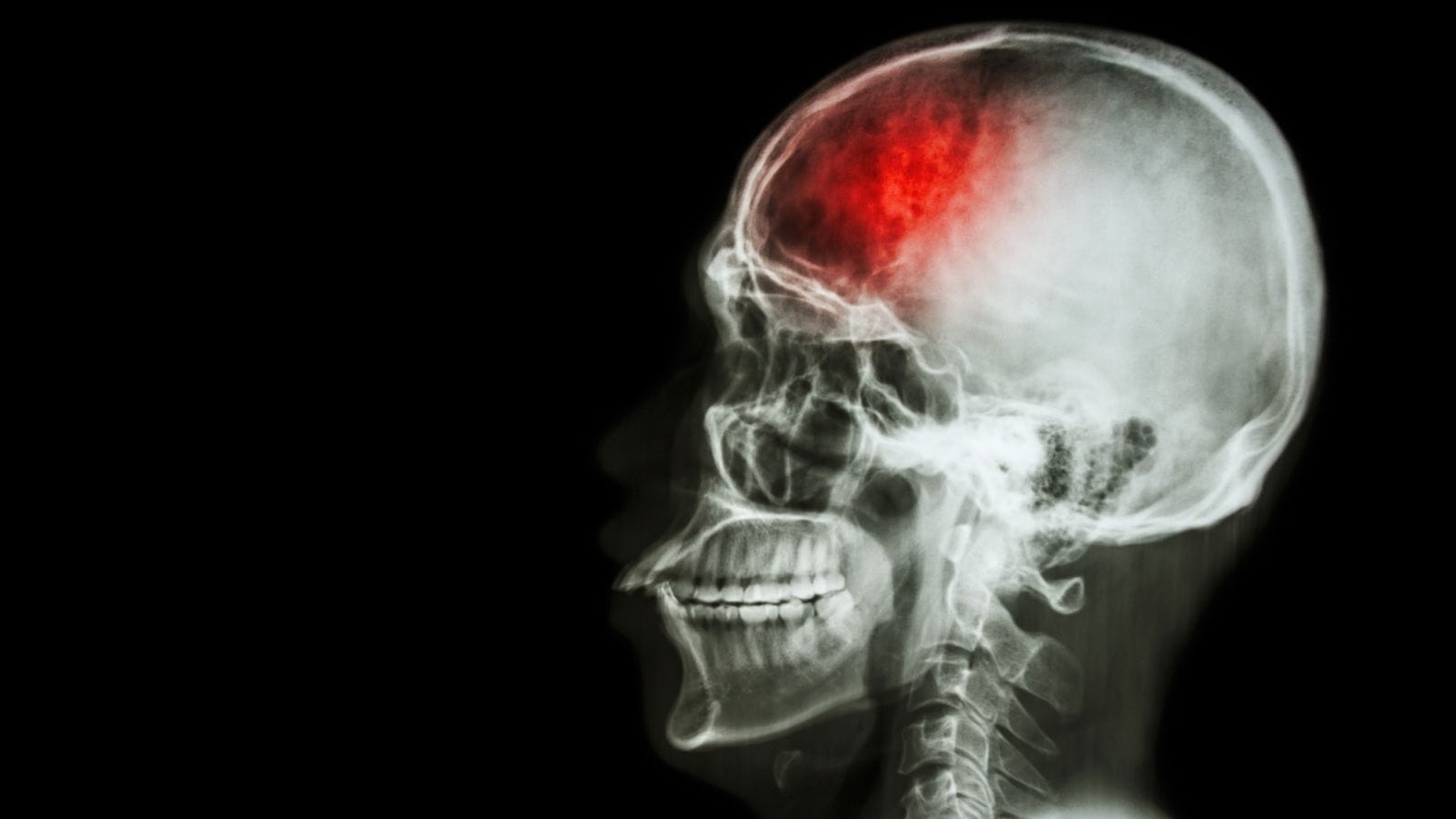
Atrial Fibrillation (AF): In this arrhythmia, the risk of clot formation in the heart increases. If a clot travels to the brain, it may cause a stroke. Therefore, blood thinners are often essential in AF patients.
Deep Vein Thrombosis (DVT) and Pulmonary Embolism: Clots in deep veins, especially in the legs, can travel to the lungs and cause life-threatening embolism. Blood thinners prevent existing clots from growing or new ones from forming.
Heart Valve Prostheses: Patients with mechanical heart valves are at high risk for clot formation around the valve, so they may need lifelong or long-term anticoagulant use.
After Heart Attack: Blood thinners are used to minimize the risk of a new heart attack, especially where heart muscle damage increases clot risk.
Stroke (Ischemic): In some types of stroke, blood thinners help prevent or reduce the risk of recurrence.
Certain Hereditary Clotting Disorders and Other High-Risk Situations: Blood thinners may be prescribed for genetically clot-prone individuals or as prevention after major surgeries.
In general, blood thinners act as insurance to prevent the formation of life-threatening clots. Just as you’d build a barrier to prevent flooding in your house, these medications are used when the risk is high, even if you can’t predict exactly when a clot might form.
How Do Blood Thinners Work?
Blood thinners work via two main mechanisms:
Anticoagulants:
Warfarin: Inhibits the production of certain clotting factors in the liver, especially those dependent on vitamin K, thus slowing clot formation.
Heparin and Low Molecular Weight Heparins (LMWH, e.g., enoxaparin): Enhance the natural action of antithrombin, inactivating key enzymes like thrombin and factor Xa.
DOACs (Dabigatran, Rivaroxaban, Apixaban, Edoxaban): Some directly block thrombin, others block factor Xa. They are considered “more technological” with more predictable effects and less need for regular blood tests.
Antiplatelet Drugs:
Aspirin (ASA): Blocks the production of thromboxane A2 in platelets, making it harder for them to stick together.
Clopidogrel, Prasugrel, Ticagrelor: Block ADP receptors on platelets, reducing their ability to clump and form clots.
Think of these drugs as “traffic police” for the circulatory system, controlling or slowing the flow where necessary to prevent “traffic accidents” (unwanted clots).
Which Blood Thinners Are Most Commonly Used?
Although there are many types, the most frequently used blood thinners are:
Warfarin (Coumadin):
- Classic anticoagulant in use for many years.
- Requires precise dose adjustments and frequent blood (INR) tests.
- Can interact with dietary vitamin K (e.g., spinach, broccoli).
Heparin (Unfractionated Heparin, UFH):
- Administered intravenously or subcutaneously, often in hospitals for rapid effect.
- Used in intensive care or around surgeries.
- Dose is monitored with blood tests (aPTT).
Low Molecular Weight Heparins (LMWH; Enoxaparin, Dalteparin):
- Predictable effect, generally once or twice daily injection.
- Can be used outside the hospital in some cases.
- Less intensive blood test monitoring than UFH.
DOACs (Dabigatran, Rivaroxaban, Apixaban, Edoxaban):
- Newer generation oral blood thinners with stable effects and less need for regular tests.
- Often have a better side effect profile than warfarin in certain patients.
Aspirin and Other Antiplatelet Drugs (Clopidogrel, etc.):
- Mainly for reducing heart attack or stroke risk, sometimes after stent placement.
- Usually low-dose, once daily (e.g., 75–100 mg).
- May increase the risk of bleeding in the stomach or intestines.
Choice of drug, dosing, and duration depend on the patient’s clinical condition.
Why Are Blood Thinners So Important?
Blood thinners are like “life insurance” for those with cardiovascular disease. A clot inside a vessel can block blood flow, just as a fallen branch blocks a road. Blockage in a brain vessel causes stroke; in a heart vessel, heart attack; in a leg vessel, DVT.
Because sudden clots can lead to severe disability or death, blood thinners are recommended for high-risk individuals. They “put the brakes” on the clotting system without shutting it down entirely. Without this balance, even small injuries would cause unstoppable bleeding, so individual dosing and choice of medication is key.
What Are the Possible Side Effects of Blood Thinners?
The most common side effect is, naturally, an increased risk of bleeding. For example:
Minor Bleeding: Gum bleeding, nosebleeds, easy bruising.
Serious Bleeding: Excessive bleeding in internal organs (such as the brain, GI tract) or at surgery sites.
Other Side Effects:
- Warfarin: Rarely, skin necrosis or “purple toe syndrome.”
- Heparin: “Heparin-induced thrombocytopenia (HIT),” which paradoxically increases clot risk.
- DOACs: Rarely, liver dysfunction or allergic reactions.
- Long-term warfarin use: Increased risk of osteoporosis and fractures.
The degree of bleeding risk depends on the drug type, patient’s other illnesses, age, and additional medications. For example, using stomach-protective drugs with aspirin can lower GI bleeding risk.
What Should Be Considered While Using Blood Thinners?
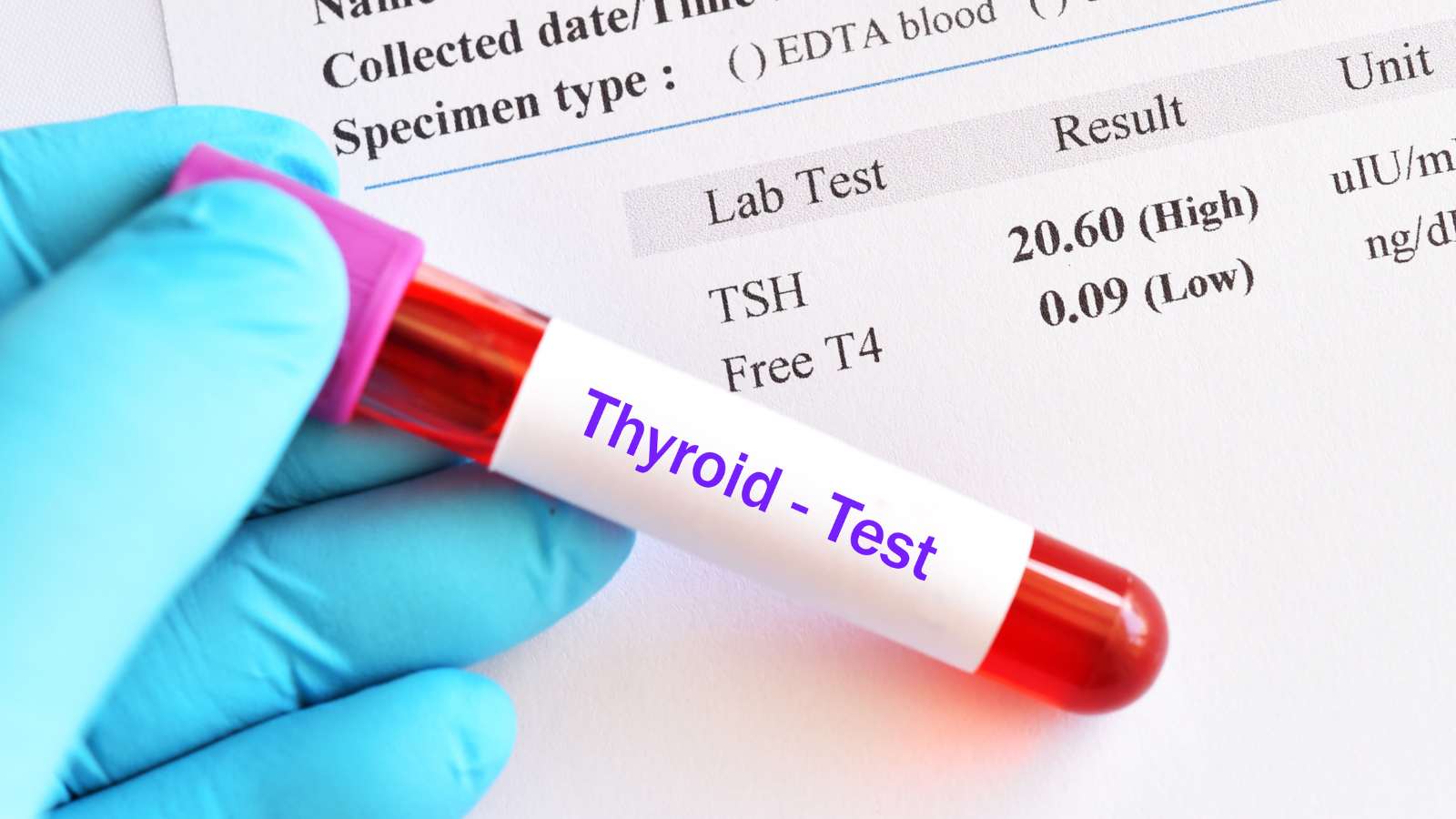
Regular Monitoring:
- Patients on warfarin must have regular INR blood tests. High values mean bleeding risk; low values mean clot risk.
- DOACs usually do not require routine testing, but kidney and liver function should be checked periodically.
Diet and Nutrition:
- Those on warfarin should avoid sudden changes in vitamin K intake. For example, eating lots of spinach regularly and then stopping suddenly can cause major INR swings.
- Alcohol increases the effect of blood thinners and the risk of bleeding, so use cautiously.
Other Drugs and Supplements:
- Certain drugs (painkillers, antibiotics, statins, stomach meds) can interact with blood thinners. Always inform your doctor about new medications.
- Herbal supplements (ginger, garlic, ginkgo biloba, etc.) can unexpectedly increase bleeding risk. Always seek medical advice before use.
Avoiding Falls and Injuries:
- Take precautions to prevent injuries, especially to the head. Use non-slip mats and grab bars at home.
Recognizing Bleeding Symptoms:
- Blood in urine, black or red stool, excessive bruising, unexplained fatigue, or dizziness may indicate internal bleeding and require immediate medical attention.
Are There Natural Blood Thinners?
Some foods and herbs have mild natural blood-thinning effects, such as:
- Ginger, garlic, turmeric (curcumin), olive oil, onion.
- Fermented products like nattokinase may help break down fibrin.
However, their effects are much weaker and less standardized than prescription drugs, and they may interact with medical therapy, unexpectedly increasing bleeding risk. For example, excessive garlic can interact with warfarin and cause bleeding. Always consult a physician before using any natural supplements.
Can Blood Thinners Be Used During Pregnancy and Breastfeeding?
Blood thinners during pregnancy and breastfeeding should only be used under specialist supervision. Some anticoagulants, especially warfarin, can harm the baby and cross the placenta. Therefore, warfarin is generally avoided in pregnancy.
- Low molecular weight heparins (LMWH) are usually considered safer in pregnancy since they do not cross the placenta.
- DOACs are generally not recommended due to limited data.
- During breastfeeding, LMWH is usually safe, and warfarin can sometimes be used in low doses, but always with medical approval.
Close monitoring and regular blood tests are important to protect both mother and baby during these periods.
How Do Blood Thinners Interact With Other Drugs?
Blood thinners can interact with many drugs. For example:
- Warfarin interacts with many drugs metabolized by the liver (antibiotics, antidepressants, painkillers, thyroid drugs, etc.).
- DOACs can interact with some antiviral and antifungal medications.
- Aspirin and other antiplatelet drugs increase GI bleeding risk when used with corticosteroids or NSAIDs.
Proton pump inhibitors (PPIs) may reduce the effectiveness of clopidogrel, although this does not affect all patients equally. Physicians always consider drug interactions when prescribing.
How Are Blood Thinners Managed Before Surgery or Dental Procedures?
Blood thinners may need to be stopped or the dose adjusted before surgery or dental procedures to reduce bleeding risk. The timing depends on the drug and patient’s health:
Warfarin: Usually stopped 5 days before the procedure; INR should return to normal. High-risk patients may receive bridging with heparin.
DOACs: Usually stopped 24–48 hours prior, depending on kidney function and drug half-life.
Heparin (UFH or LMWH): Last dose is typically withheld 12–24 hours before the procedure.
Antiplatelet drugs: Aspirin is usually stopped 7–10 days before, but do not stop without consulting your doctor, especially in heart disease or stent patients.
After surgery, restarting blood thinners as soon as bleeding is controlled is essential, with careful monitoring.
Can Blood Thinners Be Used Long-Term?
Duration of blood thinner use depends on the underlying condition and risk of clotting:
- For temporary risks (e.g., after a leg fracture), 3–6 months may be sufficient.
- For chronic atrial fibrillation or mechanical heart valves, lifelong therapy is often necessary.
- For recurrent VTE or hereditary clotting disorders, long-term or permanent therapy may be needed.
The decision is always made jointly by the patient and doctor, weighing the risks of clotting versus bleeding.
Is It Safe to Stop or Adjust Blood Thinners on Your Own?
Blood thinners should never be stopped or dose-adjusted without medical advice. Suddenly stopping these drugs can cause serious complications. For example, stopping anticoagulants in AF patients greatly increases stroke risk. Incorrect dosing also increases the risk of bleeding or new clots. Always make changes under medical supervision.
FAQ
Is alcohol completely prohibited when using blood thinners?
Not absolutely, but excessive alcohol increases bleeding risk. Consume in moderation and follow your doctor’s recommendations.
Do herbal teas interact with blood thinners?
Some herbs (e.g., green tea, ginger, ginkgo biloba) have blood-thinning effects and may enhance the effect of your medication. Always consult your doctor.
Can people on blood thinners have dental procedures?
Yes, but always inform your dentist. Some adjustments may be necessary, and bleeding risk should be closely monitored.
What if someone wants to become pregnant while on blood thinners?
Medication adjustments may be necessary for planned pregnancy. Warfarin is usually not preferred during pregnancy due to risks for the baby. Always decide with your physician.
Are blood thinners used in the treatment of varicose veins?
Varicose veins alone do not always require blood thinners. However, if varicose veins increase the risk of clots in the legs, temporary or permanent anticoagulation may be considered.

Interventional Radiology and Neuroradiology Speaclist Prof. Dr. Özgür Kılıçkesmez graduated from Cerrahpaşa Medical Faculty in 1997. He completed his specialization at Istanbul Education and Research Hospital. He received training in interventional radiology and oncology in London. He founded the interventional radiology department at Istanbul Çam and Sakura City Hospital and became a professor in 2020. He holds many international awards and certificates, has over 150 scientific publications, and has been cited more than 1500 times. He is currently working at Medicana Ataköy Hospital.






Vaka Örnekleri