Subdural hemorrhage is bleeding between the dura mater and the brain surface, usually caused by head trauma. It can develop acutely or chronically, leading to increased intracranial pressure and neurological impairment.
Acute subdural hemorrhage presents with headache, vomiting, and loss of consciousness. Chronic cases may show confusion, memory loss, and gradual neurological decline, especially in elderly patients.
Diagnosis is confirmed with CT or MRI imaging. These modalities identify the extent of bleeding, brain compression, and guide the urgency of neurosurgical intervention.
Treatment options include surgical evacuation via craniotomy or burr hole drainage. Close monitoring in intensive care is essential, as untreated subdural hemorrhage can be fatal.
| Disease Name | Subdural Hemorrhage |
| Definition | Bleeding that occurs between the surface of the brain and the dura mater (the outermost layer of the brain); it usually develops as a result of head trauma, and the bleeding may progress slowly. |
| Symptoms | Headache, nausea, vomiting, confusion, drowsiness, neurological disorders (speech, movement difficulties), personality changes, and in severe cases, coma and loss of consciousness. |
| Causes | Head trauma, minor traumas in the elderly, brain tissue shrinkage with age, use of blood thinners, alcoholism, bleeding disorders. |
| Risk Factors | Advanced age, those at high risk of falling, use of anticoagulant (blood thinning) medications, alcohol dependency, history of recurrent head trauma. |
| Diagnostic Methods | Brain CT (computed tomography), MRI (magnetic resonance imaging), which provides detailed examination especially in chronic subdural hemorrhages. |
| Treatment Methods | Observation for small and asymptomatic bleeds; surgical evacuation (craniotomy or burr hole evacuation of the hematoma) for symptomatic or large bleeds, monitoring blood pressure and neurological status, ventilator support if necessary. |
| Complications | Increased pressure on brain tissue, neurological disorders, permanent brain damage, brain herniation, death. |
| Surgical Requirement | Emergency surgery may be necessary for significant or progressive symptoms to evacuate the hematoma; burr hole or craniotomy is applied. |
| Recovery Time | Varies depending on the extent of damage and treatment; may take weeks to months, with possible permanent neurological sequelae in some cases. |
| Prevention Methods | Reducing the risk of falls (especially for the elderly, home safety measures), preventing head trauma, use of helmets, using anticoagulant treatment under medical supervision. |
Prof. Dr. Özgür KILIÇKESMEZ Prof. Dr. Kılıçkesmez holds the Turkish Radiology Competency Certificate, the Turkish Interventional Radiology Competency Certificate, Stroke Treatment Certification, and the European Board of Interventional Radiology (EBIR). In his academic career, he won the Siemens Radiology First Prize in 2008.
Interventional Radiology / Interventional Neuroradiology
What is Subdural Hemorrhage?
Subdural hemorrhage is the leakage of blood between the dura mater and the arachnoid membrane. It usually results from tearing of the bridging veins in the brain due to head trauma. Depending on the duration and characteristics of the bleeding, it is called acute, subacute, or chronic. Acute subdural hemorrhage develops rapidly and often causes a sudden deterioration in neurological symptoms. Chronic subdural hemorrhage, however, accumulates slowly over weeks, leading to more gradual progression of symptoms. While traumatic brain injuries are the most common cause, it may also occur spontaneously in individuals with bleeding disorders. The risk of bleeding is higher in those receiving anticoagulant therapy, which requires careful monitoring.
What Are the Causes of Subdural Hemorrhage?
Subdural hemorrhage is a collection of blood caused by the tearing of vessels around the brain and can be triggered by various factors. Head trauma is the most prominent, especially since even minor falls can cause bleeding in older adults. The aging process also increases the risk, as brain shrinkage makes the bridging veins more fragile.
Some medications can also increase the risk of bleeding. People using anticoagulant and antiplatelet drugs are more likely to develop subdural hemorrhage because of impaired blood clotting. In addition, chronic alcohol consumption in those with alcohol dependency may cause clotting problems and raise the risk.
Other factors that increase the risk of subdural hemorrhage include:
- Underlying medical conditions: Disorders such as cerebral amyloid angiopathy make individuals prone to subdural hemorrhage even after minor trauma.
- Hydrocephalus: This condition, which causes enlargement of the brain, may lead to stretching and tearing of blood vessels.
- Pathophysiological factors: Inflammation and neovascularization, especially in chronic subdural hematomas, may trigger bleeding.
- Genetic factors: Genetic conditions such as connective tissue disorders can increase the risk of subdural hemorrhage in young children.
- High-energy sports or activities: Individuals involved in high-risk activities are more likely to experience head trauma and consequently subdural hemorrhage.
*We recommend filling out all fields so we can respond in the best possible way.
How Common Is Subdural Hemorrhage?
Subdural hemorrhage (SDH) is an important health problem with different prevalence rates depending on age and gender. Each year, approximately 125,000 people in the United States are affected by SDH, and this rate increases significantly in the elderly population. The annual incidence in the general population is 13.5 per 100,000 people; in those aged 80 and above, it rises to 127.1 per 100,000. The elderly are at significantly higher risk for SDH. Chronic subdural hematoma (CSDH) is a common form of SDH, with varying incidence rates in different demographic groups.
- The incidence of CSDH varies between 1.7 and 48 cases per 100,000.
- In North Wales, from 1999 to 2017, the incidence in those over 65 increased from 8.2 to 48 per 100,000.
Age is the biggest risk factor for developing SDH. Brain atrophy, increased frequency of falls, and use of anticoagulants are factors that increase SDH incidence, especially in those over 65. Studies report higher incidence rates in elderly men over 90. Gender also affects SDH prevalence, with men having a higher incidence than women. For example, studies in Finland have shown an increase in SDH incidence in elderly men between 1990 and 2015. Demographic factors such as age and gender directly affect the prevalence of SDH.
How Does Subdural Hemorrhage Develop?
The process of subdural hemorrhage begins with the tearing of bridging veins due to trauma. This is more common in elderly individuals due to age-related brain atrophy. This atrophy creates a wider space between the dura mater and brain, increasing the vessels’ susceptibility to injury. After the initial bleed, an inflammatory response occurs, involving the migration of immune cells such as eosinophils, macrophages, and lymphocytes to the injury site. Inflammatory mediators such as interleukins and TNF-α contribute to and increase inflammation.
As bleeding progresses, a membrane begins to form around the hematoma. This membrane formation involves fibroblast differentiation and becomes a double-layered structure formed by collagen and inflammatory cells. The outer membrane is vascularized and sustains microbleeds, perpetuating bleeding and inflammation. Angiogenesis, the formation of new blood vessels, plays a critical role in subdural hematoma. The increased permeability of these new vessels allows plasma and blood cells to leak into the subdural space.
As this process continues, various structural changes occur in the hematoma and surrounding tissues:
- Collagen accumulation causes thickening of the membrane.
- Inflammation-supporting factors spread to surrounding tissue.
- These structural changes sustain a continuous cycle of inflammation and bleeding.
What Are the Symptoms of Subdural Hematoma?
Subdural hematoma presents with various symptoms, which vary depending on the severity and progression of the bleeding. Common symptoms include headaches that are mild at first but worsen over time, confusion, and drowsiness. In advanced stages, these symptoms can progress to loss of consciousness and even coma. In addition, focal neurological deficits such as weakness or numbness on one side may develop, manifesting as gait disturbances. Speech difficulties and visual problems are also frequent. Seizures may be seen in more severe cases. Acute subdural hematoma is associated with rapidly developing symptoms due to increased intracranial pressure, whereas chronic subdural hematoma usually develops slowly over weeks or months. Therefore, symptoms may vary from case to case, and clinical observation is important.
How Is Subdural Hematoma Diagnosed?
The diagnosis of subdural hematoma (SDH) relies heavily on clinical findings and neuroimaging methods. Acute, subacute, and chronic hematomas are evaluated based on symptoms and imaging findings. Clinically, symptoms such as headache, altered consciousness, and neurological deficits after head trauma are significant. Neuroimaging methods include computed tomography (CT) and magnetic resonance imaging (MRI). The diagnostic roles of these methods are as follows:
- CT Scan: Used for rapid diagnosis of acute SDH and reveals crescent-shaped hyperdense areas between the dura and the brain. In chronic cases, the hematoma may appear hypodense.
- MRI: Provides more detailed imaging for subacute or chronic SDH and is preferred when clinical findings are not clear.
How Is Subdural Hematoma Treated?
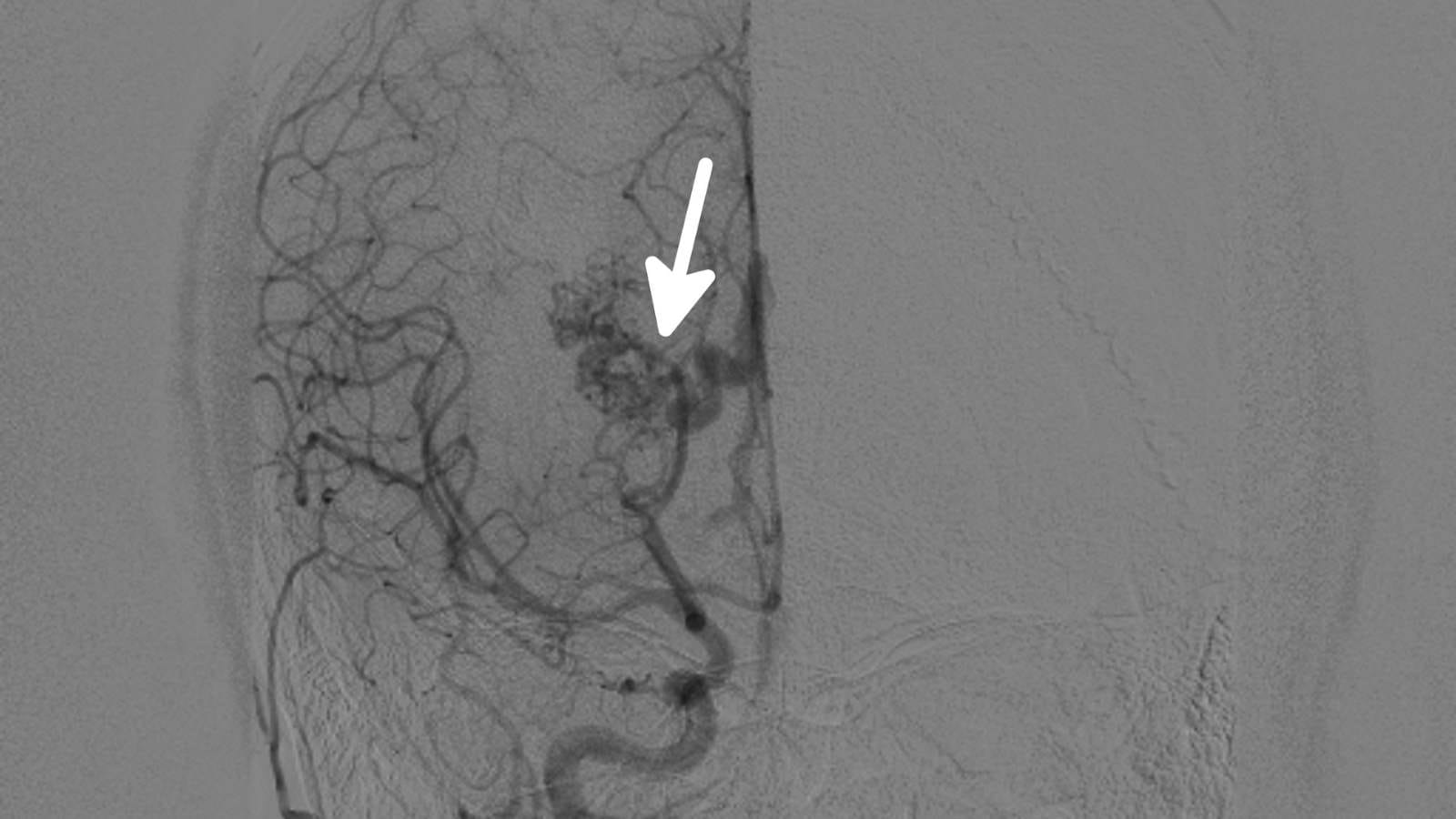
In the treatment of subdural hematoma, especially in chronic subdural hematoma (cSDH), Middle Meningeal Artery (MMA) embolization is a prominent method. This minimally invasive procedure targets the blood supply of newly formed vessels in the subdural space, aiming to stop the bleeding. The main goal is to control the bleeding, support resorption of the hematoma, and reduce recurrence rates.
Studies have shown that MMA embolization can be used both as a standalone treatment and as an adjunct to surgery. Its lower recurrence rates compared to conventional burr-hole craniotomy have increased its preference. Embolic agents used in MMA embolization include Onyx and polyvinyl alcohol (PVA) particles. Onyx, in particular, provides better results in reducing recurrence rates.
MMA embolization offers a significant advantage for patients on anticoagulant or antiplatelet therapy, as it allows continuation of these medications and prevents complications related to their withdrawal. Especially for elderly or medically complex patients, this option reduces the risk of surgical complications.
Other advantages of MMA embolization over surgical intervention include:
- Lower risk of complications
- Shorter hospital stay
- More favorable postoperative recovery profile
However, surgical intervention may still be necessary for large hematomas or those with significant midline shift. Therefore, proper patient selection and treatment method are important.
What Are the Risk Factors for Subdural Hematoma?
There are various risk factors for subdural hematoma, which may be traumatic or non-traumatic. Elderly individuals are at higher risk due to brain atrophy. Additionally, people receiving anticoagulant or antiplatelet therapy have increased risk, as these drugs impair blood clotting. Head trauma, especially in older adults, may lead to SDH. Chronic alcohol consumption increases risk by causing brain atrophy and coagulopathy. Bleeding disorders that cause coagulopathy also raise the likelihood of subdural hematoma. Other risk factors include:
- Cerebral amyloid angiopathy, particularly associated with spontaneous SDH in the elderly.
- Chronic hypertension and cerebrovascular diseases may contribute to the development of subdural hematoma.
When Can Subdural Hematoma Be Treated?
Treatment of subdural hematoma is generally evaluated based on the patient’s condition, hematoma size, and recurrence risk. Especially for elderly patients or those receiving anticoagulant therapy, alternative treatment options may be preferred due to high surgical risks. Middle meningeal artery embolization (MMAE) is one of these methods and plays a significant role in managing chronic subdural hematomas. The main indications for MMAE include:
- Prevention of Recurrence: MMAE is used effectively to reduce recurrence risk in cases with a high rate of hematoma recurrence after surgery. Studies show that it significantly decreases rebleeding rates when combined with surgery.
- High Surgical Risk Patients: MMA embolization is an important option for patients at high surgical risk, such as the elderly or those on anticoagulant therapy. These patients can avoid complications that may arise from discontinuing anticoagulants.
- Mild to Moderate Hematomas: MMAE is generally considered more suitable for hematomas with a thickness of less than 18 mm and a midline shift of less than 5 mm. In such cases, the risk of neurological damage is minimal and large surgical procedures can be avoided.
- Adjunct to Surgery: MMAE may be used after surgical intervention to prevent recurrence of the hematoma. Embolization of feeding vessels in the postoperative period reduces the likelihood of recurrence.
When Can Subdural Hematoma Not Be Treated?
In some cases, interventional radiology methods may not be appropriate in the treatment of subdural hematoma. Middle meningeal artery embolization (MMAE) carries significant risks for some patient groups and may be contraindicated in certain clinical situations. The main situations in which MMAE cannot be performed are listed below:
- Coagulopathies and Thrombocytopenia: MMAE is generally not recommended in patients with thrombocytopenia (platelet count <75,000/µl) or refractory coagulopathies due to the risk of hematoma expansion. In particular, coagulopathies associated with cancer complicate management without careful observation.
- Concurrent Antiplatelet or Anticoagulant Therapy: Discontinuing antithrombotic therapy may increase the risk of ischemic events. While MMAE allows continuation in some cases, high-risk anticoagulant use requires careful risk management.
- Technical Factors: It may be difficult to perform MMAE in elderly patients or those with difficult vascular access. For example, radial access may be preferred over femoral, but vessel tortuosity or spasm can limit this.
- Severe Neurological Impairment: In patients with severe brain injury or deep coma, the chance of recovery is low, and MMAE is considered contraindicated. In such cases, palliative care is often more appropriate.
- Active Infections: In patients with active infection or sepsis, invasive procedures such as MMAE increase the risk of systemic infection. Therefore, interventions are avoided during active infection.
What Is the Recovery Process After Subdural Hematoma Treatment?
The recovery process after subdural hematoma treatment is quite complex and depends on various factors. First, patients are closely monitored for postoperative complications. Common complications include seizures, infections, and risk of recurrent bleeding. The use of prophylactic anticonvulsants varies by institution. Delayed awakening from coma and cerebral hyperperfusion are also more common in severe cases. Elderly patients are at greater risk of developing delirium, leading to longer hospital stays.
- Recurrence and retreatment: Hematoma recurs in 10–20% of patients after surgical evacuation. Interventional radiology methods such as MMA embolization show promising results in reducing recurrence rates. Occlusion of the middle meningeal artery cuts off blood flow to the hematoma capsule and decreases the risk of recurrence.
- Functional recovery: Many patients show neurological improvement after subdural hematoma treatment. However, some patients may have persistent cognitive problems and movement limitations. The recovery process can be longer, especially for elderly patients and those with poor preoperative function.
How Can Subdural Hematoma Be Prevented?
Prevention of subdural hematoma is based on increasing safety in high-risk individuals and reducing the possibility of recurrence. Managing risk factors is crucial, especially for the elderly. Individuals over 65 are at higher risk due to brain atrophy and frequent falls. Addressing mobility and balance problems is important to reduce the risk of falls.
Medication management also plays a critical role in reducing the risk of subdural hematoma:
- The dosage of anticoagulant (e.g., warfarin) or antiplatelet (e.g., aspirin) medications should be carefully monitored in individuals using these drugs.
- Alternative treatment options should be considered for high-risk individuals when necessary.
Surgical innovations also provide significant benefits to reduce recurrence of subdural hematoma. Minimally invasive techniques lower the recurrence rate and support postoperative recovery. Pharmacological approaches are also important, as some medications have the potential to control bleeding and reduce inflammation, but their effectiveness continues to be evaluated by studies.
Finally, trauma prevention is a fundamental strategy to reduce acute subdural hematoma. Using protective equipment during high-risk activities and increasing home safety for elderly individuals can minimize the risk of falls. Such precautions are among the most practical strategies for protecting the health of the elderly population.

Interventional Radiology and Neuroradiology Speaclist Prof. Dr. Özgür Kılıçkesmez graduated from Cerrahpaşa Medical Faculty in 1997. He completed his specialization at Istanbul Education and Research Hospital. He received training in interventional radiology and oncology in London. He founded the interventional radiology department at Istanbul Çam and Sakura City Hospital and became a professor in 2020. He holds many international awards and certificates, has over 150 scientific publications, and has been cited more than 1500 times. He is currently working at Medicana Ataköy Hospital.







Vaka Örnekleri