Goiter is the abnormal enlargement of the thyroid gland, often caused by iodine deficiency, autoimmune disease, or nodular growth. Symptoms may include swelling in the neck, difficulty swallowing, hoarseness, and breathing problems, requiring clinical evaluation and treatment.
Symptoms of goiter vary depending on thyroid function. Hypothyroidism leads to fatigue, weight gain, and cold intolerance, while hyperthyroidism may cause weight loss, palpitations, and nervousness. Large goiters can cause visible swelling and compressive complaints.
Treatment depends on the underlying cause. Mild cases may require observation, while iodine supplementation or hormone therapy regulates thyroid function. In nodular or toxic cases, radioiodine therapy or interventional procedures may be recommended.
Surgical intervention is reserved for patients with severe compression, cosmetic concerns, or suspected malignancy. Minimally invasive alternatives such as radiofrequency ablation are increasingly used, reducing the need for extensive thyroid surgery.
| Disease Name | Goiter |
| Definition | A disease characterized by the enlargement of the thyroid gland. The enlargement may result from iodine deficiency, thyroid diseases, or immune system disorders. |
| Symptoms | Swelling in the neck (thyroid enlargement), difficulty swallowing or breathing, cough, hoarseness, and in some cases, symptoms related to thyroid hormone deficiency or excess. |
| Types of Goiter | Simple goiter (normal hormone level), toxic goiter (high hormone level), nodular goiter (nodule formation in the thyroid), multinodular goiter (containing multiple nodules). |
| Causes | Iodine deficiency, autoimmune diseases (Graves’ disease, Hashimoto’s thyroiditis), genetic factors, thyroid nodules, exposure to radiation. |
| Risk Factors | Living in regions with iodine deficiency, family history of thyroid disease, female gender, old age, pregnancy, and menopause. |
| Diagnostic Methods | Physical examination, blood tests (T3, T4, TSH), thyroid ultrasound, thyroid scintigraphy, fine-needle aspiration biopsy. |
| Treatment Methods | Iodine supplementation (if due to iodine deficiency), thyroid hormone replacement therapy, antithyroid drugs (if hyperthyroidism is present), radioactive iodine therapy, surgical intervention (thyroidectomy) for large or symptomatic goiters. New generation treatments: Radiofrequency or microwave ablation, embolization (these methods preserve the normal parts of the thyroid and eliminate the problematic areas). |
| Complications | Difficulty breathing or swallowing, vocal cord damage (post-surgery), hypothyroidism or hyperthyroidism, risk of thyroid cancer. |
| Surgical Requirement | Surgery is considered for large goiters that cause swallowing or breathing problems, cases unresponsive to medication, or in the presence of cancer suspicion. |
| Prevention Methods | Ensuring adequate iodine intake (use of iodized salt), regular thyroid gland check-ups, especially for high-risk groups. |
Prof. Dr. Özgür KILIÇKESMEZ Prof. Dr. Kılıçkesmez holds the Turkish Radiology Competency Certificate, the Turkish Interventional Radiology Competency Certificate, Stroke Treatment Certification, and the European Board of Interventional Radiology (EBIR). In his academic career, he won the Siemens Radiology First Prize in 2008.
Interventional Radiology / Interventional Neuroradiology
What Is Goiter?
Goiter is a condition that occurs when the thyroid gland becomes larger than normal. It usually develops due to various factors that can affect the proper functioning of the thyroid gland. Iodine deficiency, autoimmune diseases, and nodules developing in the thyroid gland are among the main causes of goiter. The thyroid gland produces important hormones that regulate the body’s metabolism. However, goiter may cause the gland to produce more or less of these hormones than normal. In some cases, thyroid hormone production may remain normal. This disorder is often noticeable by a distinct swelling in the neck. In advanced cases, symptoms such as difficulty breathing or swallowing may occur. The treatment method depends on the size of the goiter and the underlying cause.
What Are the Causes of Goiter?
Several factors may contribute to the development of goiter, leading to the enlargement of the thyroid gland. First, iodine deficiency is one of the most common causes of goiter worldwide. The lack of iodine, which is necessary for the production of thyroid hormones, leads to a decrease in hormone production and, as a result, enlargement of the thyroid gland.
Some autoimmune disorders are also important causes of goiter. Hashimoto’s thyroiditis is when the immune system attacks the thyroid gland, leading to decreased thyroid hormones and triggering the development of goiter. In addition, Graves’ disease, by causing excessive thyroid hormone production, can also contribute to the enlargement of the thyroid gland.
Moreover, thyroid nodules can lead to abnormal growths in the thyroid gland. Although these nodules are generally benign, they can cause the thyroid to grow irregularly. Genetic factors and environmental influences may play a role in the development of thyroid nodules.
Inflammation can also be effective in the development of goiter. Thyroiditis, infections, or the side effects of some medications may cause inflammation in the thyroid gland and disrupt the thyroid hormone balance, resulting in goiter.
How Common Is Goiter?
Goiter is a significant health problem worldwide, with varying prevalence in different regions and populations. Globally, goiter is known to affect about 15.8% of the population. Regional differences are quite striking. For example, the rate of goiter is about 4.7% in America, while in Africa, this rate can reach as high as 28.3%. The disease is especially more common in areas where iodine deficiency is prevalent.
Studies in Ethiopia have shown that the rate of goiter is especially high among school-age children. In regions with common iodine deficiency, the incidence of goiter in children can reach up to 50%. Another study emphasized that about 31% of children in Ethiopia showed symptoms of goiter. This is particularly linked to insufficient iodine intake.
- Demographic factors also have a significant effect on the prevalence of goiter.
- Age: Goiter tends to affect children aged 6-12 more. This age group is more vulnerable to iodine deficiency.
- Gender: The prevalence of goiter is higher in women than in men. However, this difference may vary depending on geography and iodine intake.
- Geographic location: Goiter is more common in mountainous and remote areas where iodine deficiency is widespread.
- Socioeconomic status: Low income levels are associated with poor nutrition and iodine deficiency.
*We recommend filling out all fields so we can respond in the best possible way.
What Is the Formation Process of Goiter?
The formation of goiter is a process characterized by the enlargement of the thyroid gland, and this growth is often based on complex mechanisms. Many factors can trigger this enlargement, and the process can progress over time, leading to different clinical pictures. The growth can be diffuse or nodular, and the severity of the disease depends on the underlying causes.
The most common cause of goiter is iodine deficiency. Iodine is a mineral necessary for the production of thyroid hormones, and when it is lacking, the thyroid gland responds more strongly to stimulating hormones from the pituitary gland due to inadequate hormone production. This process causes the gland to enlarge.
Genetic factors also play an important role in the development of goiter. Hereditary predisposition, especially in conditions such as multinodular goiter, may set the stage for the development of the disease. This genetic makeup can affect thyroid function and size, contributing to disease progression.
Certain environmental factors can also accelerate the development of goiter:
- Goitrogen-containing foods (cruciferous vegetables)
- Medications such as lithium
- Smoking
- Nutritional deficiencies (such as selenium and iron)
Autoimmune diseases are another important factor. Disorders such as Graves’ disease and Hashimoto’s thyroiditis may cause overstimulation or destruction of the thyroid gland. These conditions can lead to the growth of the gland and contribute to the development of goiter. These multifaceted causes shape the goiter formation process and influence the treatment plan.
What Are the Symptoms of Goiter?
The symptoms of goiter vary depending on the size of the thyroid gland, hormone production level, and underlying causes. Some patients may have mild symptoms, while others may experience more serious problems. Usually, a noticeable swelling or lump in the neck is the first sign. In addition, other symptoms may develop depending on the size of the goiter.
As goiter enlarges, a feeling of discomfort or fullness may occur in the neck. This discomfort is often experienced as difficulty swallowing or a sensation of something being stuck in the throat. Breathing difficulties can also be seen, especially when large goiters press on the windpipe. Difficulty breathing, wheezing, or increased shortness of breath while lying down are common symptoms.
Because the thyroid gland is close to the vocal cords, goiter can cause hoarseness or changes in the voice. In some patients, thyroid hormone imbalances may accompany goiter. In cases of hyperthyroidism, symptoms such as rapid heartbeat, weight loss, and irritability may occur. In hypothyroidism, symptoms such as fatigue, weight gain, cold intolerance, and constipation may be experienced.
- Visible swelling
- Neck discomfort
- Difficulty breathing
- Hoarseness
- Symptoms of hyperthyroidism
- Symptoms of hypothyroidism
These symptoms of goiter can significantly affect the patient’s quality of life and play an important role in determining the treatment plan.
How Is Goiter Diagnosed?
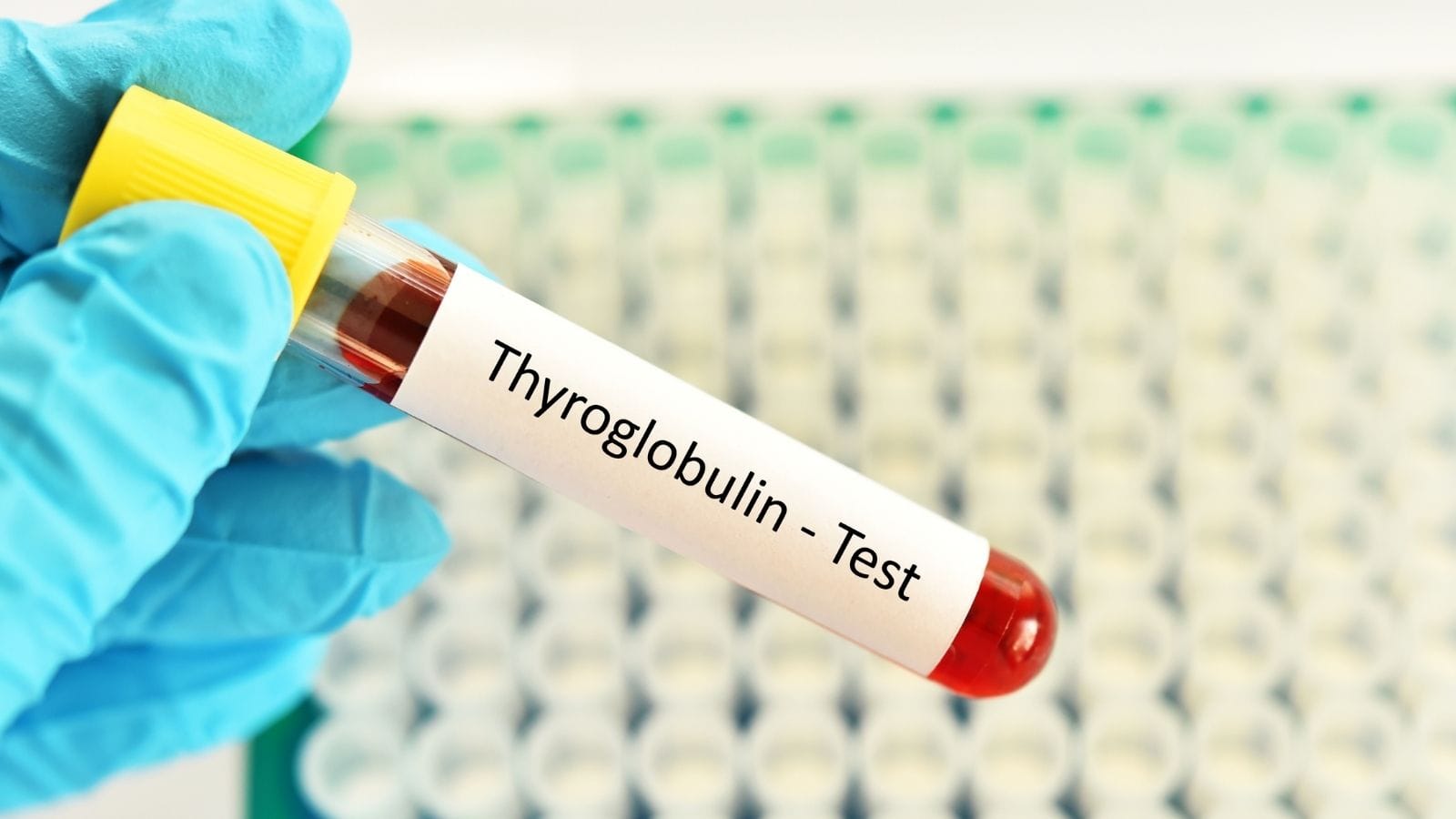
The diagnosis of goiter is a detailed process involving various methods. First, the doctor evaluates the swelling in the neck and examines the size, shape, and texture of the thyroid gland during physical examination. At this stage, it can be determined whether the goiter is diffuse or nodular. Then, blood tests measuring thyroid hormone levels (T3, T4) and Thyroid Stimulating Hormone (TSH) are performed. These tests are important to determine if goiter is related to hormonal imbalance.
Imaging techniques are used for a more detailed assessment of the size and structure of the goiter. The preferred initial method is ultrasound, which shows the structural features of thyroid nodules.
- Ultrasound: Used to evaluate the general structure of the thyroid and to distinguish cysts and nodules.
- Thyroid Scintigraphy: This imaging method uses radioactive isotopes to examine thyroid function.
- In case of suspicious nodules, fine-needle aspiration biopsy (FNAB) is performed. This procedure is done to determine malignancy in nodules with a risk of cancer.
- FNAB Biopsy: A small sample is taken from the thyroid tissue under ultrasound guidance.
In advanced cases, especially goiters that extend into the chest, detailed evaluation may be performed using computed tomography (CT) and magnetic resonance (MR) scans. In addition, the radioactive iodine uptake test (RAIU) measures the iodine uptake capacity of the thyroid gland.
How Is Goiter Treated?
In recent years, minimally invasive methods have come to the forefront as alternatives to traditional surgery in the treatment of goiter. Interventional radiology plays an important role in this field. These methods offer patients less risk and a faster recovery process, making them preferable. The following techniques are widely used, especially in the treatment of nodular goiter:
- Thyroid Artery Embolization (TAE): TAE is a technique that reduces goiter size by blocking blood flow to the thyroid gland. It is performed under local anesthesia and often preserves thyroid function.
- Radiofrequency Ablation (RFA): RFA uses radio waves to heat and destroy abnormal tissue in thyroid nodules. It is used to shrink nodules and relieve symptoms caused by goiter.
- Microwave Ablation (MWA): MWA uses microwave energy to ablate thyroid tissue by heating. It is particularly effective for large nodules and is a promising option for patients who are not suitable for surgery.
Each of these techniques aims to avoid the complications of surgery and offer patients a more comfortable treatment process. In addition, these methods do not require large incisions and allow patients to return to daily life quickly due to short recovery times.
What Are the Risk Factors for Goiter?
Many factors can be effective in the development of goiter, and some individuals are at higher risk for this disease. Iodine deficiency is the most common cause of goiter worldwide. When the thyroid gland does not receive enough iodine, it begins to enlarge. Especially women are more prone to goiter due to hormonal changes. Pregnancy, menopause, and menstruation are periods when this risk increases. The likelihood of goiter increases with age. Thyroid dysfunction is more common in older individuals.
Genetic predisposition is also an important factor that increases the risk of goiter. Individuals with a family history of autoimmune thyroid diseases are at higher risk of developing goiter. Environmental and dietary factors can also predispose to goiter. Selenium and iron deficiency, in addition to iodine deficiency, are among the risk factors. Goitrogenic substances found in some foods may also adversely affect the thyroid gland.
Another important risk factor for goiter is exposure to radiation. Radiation exposure during childhood or medical treatments may damage the thyroid gland. Additionally, obesity is another factor associated with thyroid enlargement. High body mass index can affect metabolic processes and contribute to goiter.
When Can Goiter Be Treated?
Goiter treatment is determined according to the patient’s condition, the size of the goiter, and the underlying causes. This treatment is generally required in certain situations and is planned according to the doctor’s recommendations. When making a decision about treatment, the patient’s overall health, the size of the goiter, and the pressure on surrounding tissues are considered.
Goiter treatment may be required in the following situations:
- Large goiters extending into the chest cavity: If the goiter is very large and progresses toward the chest, it may cause difficulty breathing and swallowing. In this case, non-surgical treatment options or interventional radiology methods may be preferred.
- Nodular goiters resistant to other treatments: If medication is ineffective or other minimally invasive techniques are not suitable, treatment is necessary. Intervention may be possible if these goiters have grown significantly and are causing pressure symptoms.
- When it is necessary to preserve thyroid function: If it is desired to preserve part of the thyroid gland instead of removing it completely, certain treatment methods may be preferred. In this way, a portion of the thyroid gland can continue to function.
- Patients unsuitable for surgery: Non-surgical methods are preferred for patients at surgical risk due to advanced age or other health problems. In such cases, less invasive techniques may provide comfort to the patient.
When Can’t Goiter Be Treated?
In some cases, goiter treatment cannot be applied. Therefore, patients’ conditions should be carefully evaluated. During interventional radiology treatment, the following contraindications should be considered:
- Severe thyroid dysfunction: Patients with poorly controlled hyperthyroidism or hypothyroidism are at risk of complications. These conditions should be managed first.
- Large substernal or retrosternal goiters: Goiters extending into the mediastinum limit treatment potential. The treatment process may become more difficult due to access issues.
- Suspicion or confirmation of malignancy: If thyroid cancer is suspected, interventional methods are not recommended. Surgical methods should be preferred in this situation.
- Severe cardiopulmonary compromise: Patients with significant cardiopulmonary disorders are at high risk. This may affect the safety of procedures.
- Infection or bleeding disorders: Active infection or bleeding disorders are contraindications for treatment.
- Pregnancy and breastfeeding: Interventions should be avoided during pregnancy due to radiation and certain medications.
- Severe allergy to contrast agents: Known allergy can negatively affect the treatment process.
What Is the Recovery Process After Goiter Treatment?
The recovery process after goiter treatment is usually faster with the application of minimally invasive methods. This positively affects the time patients return to daily life. After the procedures, patients usually experience the following:
- Recovery time: Procedures such as TAE and RFA are performed under local anesthesia. As a result, patients can return to normal activities very quickly.
- Postoperative symptoms: Patients may feel mild pain or swelling at the treatment site, but these symptoms are generally short-lived.
- Monitoring and follow-up: Monitoring thyroid function after treatment is important. Follow-up appointments help evaluate treatment effectiveness.
- Complications and management: The risk of complications after invasive procedures is low. Temporary hoarseness is rarely seen.
Recovery may vary depending on the nature of the treatment method. In general, after minimally invasive methods, patients experience less discomfort than traditional surgery. This has a positive effect on both physical and psychological well-being, allowing patients to adapt to daily life more quickly. Monitoring and management of this recovery process is important for the long-term evaluation of treatment outcomes.
How Can Goiter Be Prevented?
The prevention of goiter is especially aimed at eliminating iodine deficiency. First, iodization of salt is the most effective method and ensures adequate iodine intake in communities. In addition, the consumption of iodine-rich foods such as seafood, milk, and eggs should be encouraged. Thus, a balanced diet can reduce the risk of goiter. In areas where iodine deficiency is common, iodine supplements may be used. It is also important to manage the intake of goitrogenic foods. Finally, increasing the intake of minerals such as selenium and iron to improve overall nutrition provides an additional strategy for goiter prevention. These methods help reduce the prevalence of goiter.
Frequently Asked Questions

Is goiter cancer?
Goiter is the enlargement of the thyroid gland and is not a type of cancer. While most goiters are harmless, sometimes they may contain cancerous nodules. Therefore, it is important to examine for possible cancer cells within goiter.
Are thyroid and goiter the same thing?
Goiter is a condition caused by the enlargement of the thyroid gland and may be a sign of various thyroid disorders. This enlargement may occur when the thyroid gland produces too much hormone (hyperthyroidism), not enough hormone (hypothyroidism), or normal levels of hormone (euthyroidism). So, goiter actually indicates an abnormality in the thyroid gland but is not a disease itself. It is a sign that can result from different thyroid problems.
Can goiter be completely cured?
Yes, goiter can be completely treated, but the treatment method and its success depend on the cause of goiter. For example, goiters due to iodine deficiency can usually be resolved with appropriate iodine supplementation. In benign goiters, levothyroxine treatment can reduce thyroid size. In cases of multinodular goiter, surgical intervention—especially total thyroidectomy—offers an effective solution, but lifelong hormone support may be required. Radioactive iodine treatment, which targets overactive thyroid tissue, is also effective in goiters with excessive hormone secretion. The treatment method is determined according to the patient’s condition and the cause of the goiter.
Does goiter cause weight gain?
Goiter is known as enlargement of the thyroid gland, and if the thyroid is underactive, that is, if it leads to hypothyroidism, it can cause weight gain. Hypothyroidism slows down metabolism and usually results in weight increase. However, if goiter is associated with hyperthyroidism, meaning the thyroid is overactive, metabolism accelerates and this can cause weight loss. In summary, the effect of goiter on weight depends entirely on how the thyroid functions.
Does goiter cause pain?
Goiter usually does not cause pain; however, if there is thyroid inflammation, especially in cases such as De Quervain’s thyroiditis, pain may occur in the neck and goiter area. Such thyroid inflammations cause both swelling and pain. So, while most goiters are painless, discomfort and pain may be experienced in cases caused by inflammation.
Does goiter cause decreased sexual desire?
Yes, goiter can lead to decreased sexual desire. Thyroid dysfunctions that accompany goiter (such as hypothyroidism or hyperthyroidism) can disrupt the balance of sex hormones in the body and cause a drop in libido. Research shows that people with thyroid problems experience sexual dysfunction, low libido, erectile problems in men, and insufficient lubrication in women. Treating thyroid issues usually helps restore normal sexual function.
Does goiter cause irritability?
Goiter, especially when hormone production increases, can cause irritability. For instance, in conditions like Graves’ disease, when thyroid hormones are overproduced, a person may feel tense, irritable, and even restless. That’s why a hormonal imbalance due to goiter can really make a person more irritable and restless.
Is goiter detected in blood tests?
Goiter cannot be detected directly by blood test. However, blood tests that measure TSH and thyroid hormones (T3 and T4) help in understanding conditions that can lead to goiter, such as hypothyroidism or hyperthyroidism. But imaging methods such as ultrasound are generally used to confirm the presence of goiter.
What should goiter patients avoid?
People with goiter should be careful with some foods. They should avoid both excessive and insufficient intake of iodine-rich foods such as seaweed and iodized salt, as both can cause the thyroid gland to enlarge. Cruciferous vegetables such as cabbage and broccoli, soy products, and certain grains (especially millet) should also be consumed in moderation as they can affect thyroid hormone production. Cooking these foods can reduce their goitrogenic effect. Avoiding processed foods, especially those high in sugar and trans fats, is also important for thyroid health.
Can goiter be treated with medication?
Yes, some types of goiter can be treated with medication alone. If goiter is due to hypothyroidism, levothyroxine treatment can reduce thyroid size. In cases of goiter caused by hyperthyroidism, antithyroid drugs such as methimazole or propylthiouracil are used to reduce thyroid hormone production. However, the effectiveness of drug therapy depends on the cause and size of the goiter. In large or symptomatic goiter, surgical intervention or radioactive iodine therapy may also be needed.
What complaints do people with goiter have?
People with goiter often notice a noticeable swelling in the lower part of the neck. This swelling may lead to difficulty swallowing or breathing, cough, hoarseness, and a feeling of tightness in the throat. If goiter is related to thyroid hormone imbalance, additional symptoms may include:
- Hypothyroidism (underactive thyroid): fatigue, excessive sensitivity to cold, constipation, dry skin, weight gain, and depression.
- Hyperthyroidism (overactive thyroid): unexpected weight loss, rapid or irregular heartbeat, irritability, restlessness, and intolerance to heat.
- Additionally, some cases of goiter may be very small and show no symptoms at all.
Can goiter shrink with medication?
Yes, some medications can reduce the size of goiter. For example, levothyroxine treatment is used to suppress thyroid-stimulating hormone (TSH) levels and can help shrink benign goiter. Antithyroid drugs such as methimazole, used to treat overactive thyroid conditions, can also reduce goiter size. Radioactive iodine therapy is effective in significantly reducing goiter size—some studies show that goiter shrinks by 50-60% within 12 to 18 months with this treatment.

Girişimsel Radyoloji ve Nöroradyoloji Uzmanı Prof. Dr. Özgür Kılıçkesmez, 1997 yılında Cerrahpaşa Tıp Fakültesi’nden mezun oldu. Uzmanlık eğitimini İstanbul Eğitim ve Araştırma Hastanesi’nde tamamladı. Londra’da girişimsel radyoloji ve onkoloji alanında eğitim aldı. İstanbul Çam ve Sakura Şehir Hastanesi’nde girişimsel radyoloji bölümünü kurdu ve 2020 yılında profesör oldu. Çok sayıda uluslararası ödül ve sertifikaya sahip olan Kılıçkesmez’in 150’den fazla bilimsel yayını bulunmakta ve 1500’den fazla atıf almıştır. Halen Medicana Ataköy Hastanesi’nde görev yapmaktadır.






Vaka Örnekleri