Medullary thyroid cancer is a rare malignancy originating from C-cells of the thyroid gland. It accounts for about 3–4% of thyroid cancers and often produces elevated calcitonin levels, serving as a diagnostic marker.
Unlike papillary and follicular types, medullary carcinoma does not respond to radioactive iodine. Surgery is the primary treatment, usually involving total thyroidectomy and lymph node removal to prevent spread.
Some cases are linked to inherited genetic mutations, particularly MEN2 syndrome. Genetic testing and family screening are important to detect at-risk individuals early and initiate preventive measures.
Targeted therapies such as tyrosine kinase inhibitors are used in advanced cases. These treatments help slow disease progression, offering improved outcomes for patients with metastatic or recurrent disease.
| Disease Name | Medullary Thyroid Cancer (MTC) |
| Definition | A rare type of thyroid cancer originating from the parafollicular C cells of the thyroid gland; characterized by excessive production of the hormone calcitonin. |
| Symptoms | Painless swelling or mass in the neck, hoarseness, difficulty swallowing and breathing, diarrhea (due to excessive production of calcitonin), neck or throat pain. |
| Causes | Mostly associated with genetic mutations (RET proto-oncogene mutation); familial MTC may be part of Multiple Endocrine Neoplasia Type 2 (MEN2) syndrome. |
| Risk Factors | Family history of hereditary MTC, MEN2 syndrome, carriage of RET gene mutation, advanced age, female gender. |
| Diagnostic Methods | Physical examination, thyroid ultrasound, blood tests (T3, T4, TSH, calcitonin, carcinoembryonic antigen/CEA), fine-needle aspiration biopsy, genetic testing (RET mutation), CT or MRI imaging. |
| Treatment Methods | Total thyroidectomy (complete removal of the thyroid), removal of neck lymph nodes, monitoring calcitonin and CEA levels; in advanced stages, targeted therapies and chemotherapy. |
| Follow-up and Monitoring | Regular measurement of calcitonin and CEA levels after treatment, disease monitoring by neck ultrasound and CT/MRI as needed. |
| Complications | Spread of the disease to lymph nodes or distant organs (such as liver, lungs), hoarseness (after surgery), permanent hypothyroidism, risk of recurrence. |
| Prognosis | Although it can be controlled with early diagnosis, prognosis is more challenging in advanced stages. Genetic screening is important for early detection in familial cases. |
| Prevention Methods | In individuals with a family history of MTC, RET mutation screening by genetic testing can be considered, and prophylactic thyroidectomy may be recommended for high-risk individuals. |
| Associated Syndromes | Associated with Multiple Endocrine Neoplasia Type 2 (MEN2A and MEN2B) syndromes; these syndromes can also cause parathyroid and adrenal gland tumors. |
Prof. Dr. Özgür KILIÇKESMEZ Prof. Dr. Kılıçkesmez holds the Turkish Radiology Competency Certificate, the Turkish Interventional Radiology Competency Certificate, Stroke Treatment Certification, and the European Board of Interventional Radiology (EBIR). In his academic career, he won the Siemens Radiology First Prize in 2008.
Interventional Radiology / Interventional Neuroradiology
What Is Medullary Thyroid Cancer?
Medullary thyroid cancer is a rare cancer type that develops from the parafollicular C cells of the thyroid gland. Although it represents only 1–2% of thyroid cancers, it can have an aggressive course. Both sporadic cases and genetic syndromes, especially multiple endocrine neoplasia type 2 (MEN2), can lead to the disease. The cancer usually tends to spread early to lymph nodes and distant organs. Increased levels of calcitonin and carcinoembryonic antigen (CEA) play an important role in the diagnosis of medullary thyroid cancer. Treatment options are determined according to disease progression, and especially in advanced stages, targeted therapies may be preferred. RET inhibitors stand out among these therapies, offering hope.
What Are the Causes of Medullary Thyroid Cancer?
Medullary thyroid cancer (MTC) is based on two main causes: hereditary and sporadic factors. Hereditary causes account for 25% of cases and are usually associated with mutations in the RET proto-oncogene. These mutations lead to the development of genetic syndromes such as multiple endocrine neoplasia type 2 (MEN2). Autosomal dominant RET mutations have a 50% chance of being passed on to children if present in one parent. Hereditary MTC is divided into two subcategories:
- MEN2A: Individuals with this syndrome have a high probability (90%) of developing MTC. Other endocrine tumors such as pheochromocytoma and parathyroid adenomas are also common in these patients.
- MEN2B: Characterized by MTC appearing at a very young age, with nearly 100% risk. MEN2B is also associated with additional features such as mucosal neuromas and marfanoid body habitus.
Sporadic cases account for 75% of MTC and have no hereditary connection. They typically develop later in life, and although the exact cause is unknown, they are thought to result from spontaneous mutations in the RET gene or other molecular changes. Sporadic MTC is not associated with syndromes like MEN2 or other endocrine tumors.
How Common Is Medullary Thyroid Cancer?
Medullary thyroid cancer (MTC) constitutes 2–4% of all thyroid cancers and is a relatively rare cancer type. In the United States, the annual incidence rate is between 0.14 and 0.21 cases per 100,000 people. Although not common, this cancer type is responsible for 8% of deaths related to thyroid cancer. Sporadic cases make up 75% of all MTC, while the remaining 25% are hereditary cases, usually due to mutations in the RET proto-oncogene.
The demographic distribution of MTC is also notable. It is usually diagnosed between the ages of 40 and 60 and is more common in women than men. However, hereditary cases may present at an earlier age. Familial forms associated with MEN2 can be diagnosed in childhood or adolescence in families with known genetic mutations.
Geographically, the incidence of MTC does not vary greatly among different populations. However, hereditary cases are more frequently seen in families with known genetic mutations.
In general, although the prevalence of MTC is low, its more aggressive course and higher mortality rates, especially in hereditary cases, increase the risk. The lack of a geographical or environmental distribution for MTC indicates that such factors do not play a role in the development of sporadic cases.
*We recommend filling out all fields so we can respond in the best possible way.
What Is the Formation Process of Medullary Thyroid Cancer?
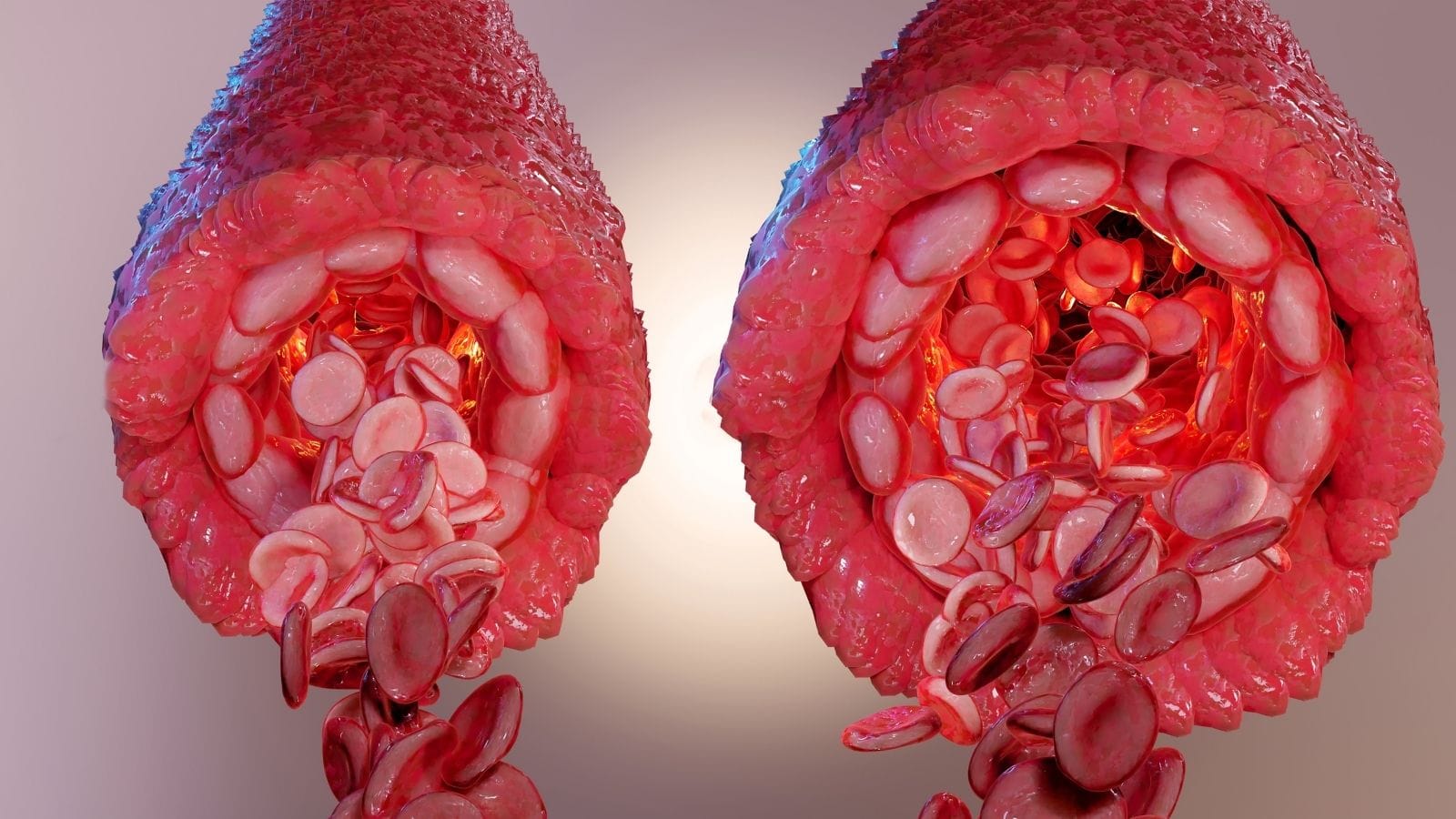
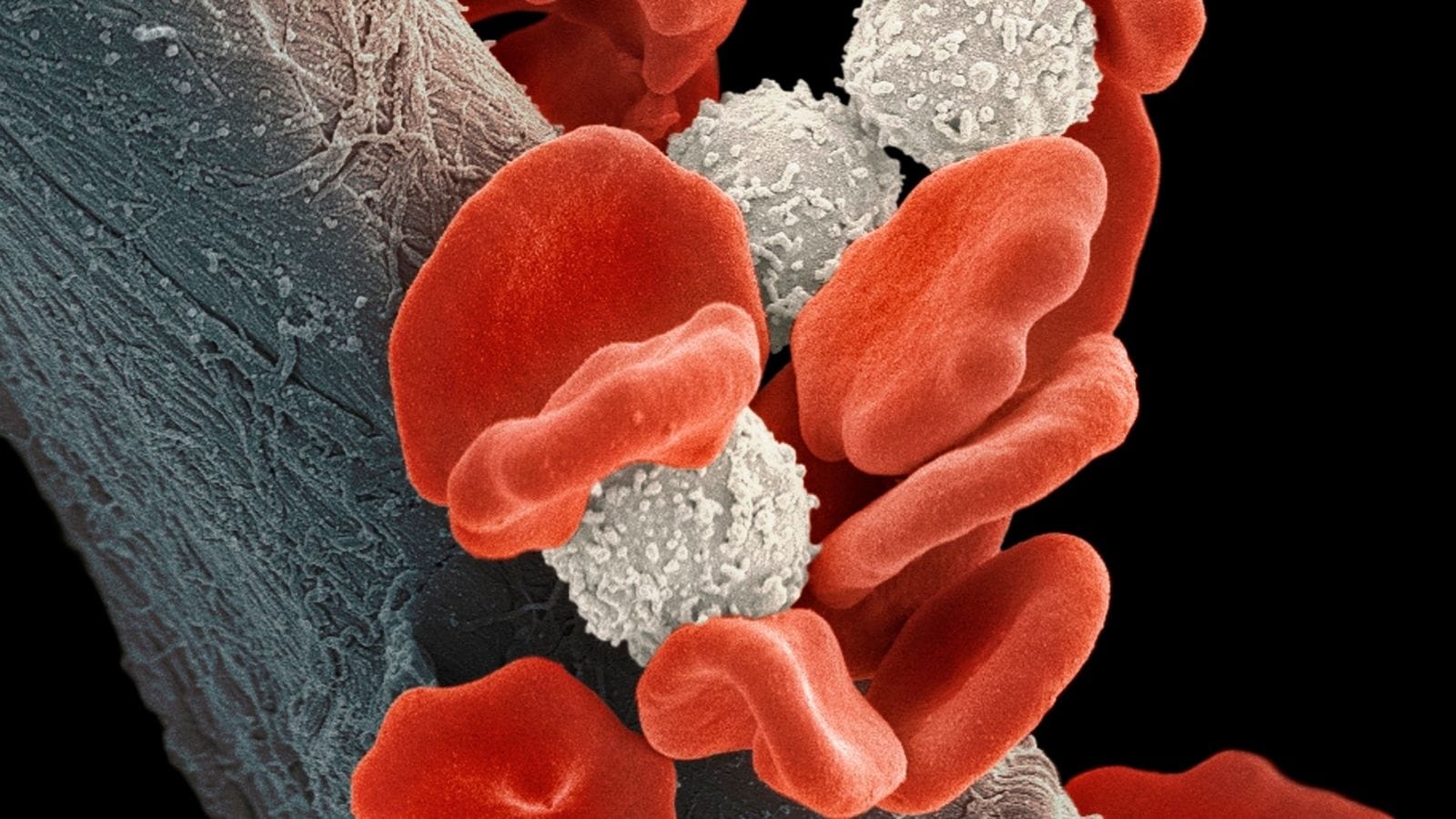
Medullary thyroid cancer (MTC) originates from the calcitonin-producing parafollicular C cells in the thyroid gland. The formation process is shaped by genetic and molecular mechanisms, which differ depending on whether the case is hereditary or sporadic. Hereditary cases mainly result from germline mutations in the RET proto-oncogene. These mutations increase tyrosine kinase activity, leading to uncontrolled cell proliferation.
In sporadic cases, somatic mutations in the RET gene are seen. Mutations outside of RET can also be important; for example, mutations in the RAS gene family can trigger cell division and proliferation. In both types, the RET proto-oncogene plays a central role in molecular pathogenesis. Constitutively active tyrosine kinase affects various signaling pathways regulating cellular growth and division.
The following signaling pathways are involved in this process:
- MAPK pathway
- PI3K-AKT pathway
Activation of these pathways supports tumor development and increases resistance to cell death. The tumor microenvironment may also cause immune cells to show weak anti-tumor activity. The low tumor mutation burden of MTC makes it easier for the tumor to evade the immune system.
As the tumor progresses and metastasizes, it can spread to lymph nodes and distant organs. This metastatic potential depends on genetic mutations and the molecular structure of the tumor. As a result, resistant cells may develop during treatment.
What Are the Symptoms of Medullary Thyroid Cancer?
Medullary thyroid cancer can present with various symptoms, which become more pronounced as the disease progresses. The most common symptom is a palpable, often painless lump or nodule in the neck. This mass is located in the upper part of the thyroid gland and may initially be asymptomatic. As the disease advances, more severe symptoms may appear.
In addition to a neck lump, the following symptoms are associated with medullary thyroid cancer:
- Neck lump: Usually the first symptom and may take time to notice.
- Swollen lymph nodes: When the cancer spreads to lymph nodes, noticeable swelling may occur in the neck.
- Hoarseness: If the tumor presses on the nerve controlling the vocal cords, hoarseness can develop.
- Difficulty swallowing or breathing: Larger tumors may press on the esophagus or trachea, causing dysphagia or dyspnea.
- Neck pain: The pain may radiate to the jaw and ears.
In advanced stages, systemic symptoms may also occur due to hormones secreted by the tumor. These usually arise in the later stages:
- Diarrhea: Frequent loose stools may result from increased calcitonin levels.
- Facial flushing: Rare, but may occur with excessive hormone secretion.
- Unexplained weight loss: Can be a severe symptom in advanced stages.
These symptoms are often mild until the cancer advances, and diagnosis is frequently delayed.
How Is Medullary Thyroid Cancer Diagnosed?
The diagnosis of medullary thyroid cancer (MTC) involves combining different evaluation methods. Initially, the patient’s clinical status provides important clues. This cancer type often presents as a thyroid nodule, causing symptoms such as difficulty swallowing, neck pain, or changes in voice. However, many patients are diagnosed incidentally during evaluations for other thyroid problems.
Serum biomarker analysis also plays a crucial role in diagnosis. Calcitonin (Ct) level is a specific indicator for MTC; levels exceeding 100 pg/mL strengthen suspicion of MTC. Carcinoembryonic antigen (CEA) levels are also used, particularly to monitor disease progression. Elevated levels of both markers suggest metastatic disease.
Genetic testing for RET proto-oncogene mutations is essential to identify hereditary forms of MTC. This test is mandatory in every patient for family risk assessment.
Fine-needle aspiration biopsy (FNAB) is a method used to diagnose thyroid nodules. Performed under ultrasound guidance, FNAB supports the diagnosis with cytological examination. Measuring calcitonin levels in the aspirate fluid obtained from the biopsy is effective for confirming the diagnosis.
How Is Medullary Thyroid Cancer Treated?
In the treatment of Medullary Thyroid Cancer (MTC), interventional radiology offers an important option when surgery or systemic treatments are not possible. These methods are especially used in advanced or metastatic disease to preserve patient quality of life and relieve symptoms. They may also provide localized control in metastatic regions and help slow disease progression.
The main interventional radiology techniques include:
- Radiofrequency Ablation (RFA): Used to shrink and control localized metastases, especially in bones, liver, and lungs to help relieve pain.
- Embolization: Cuts off blood supply to hypervascular metastatic lesions, used to reduce tumor burden in the liver and bones.
- Cryoablation: Destroys cancerous tissues by freezing; effective for pain control and slowing metastasis growth, especially in bone and lung metastases.
- External Beam Radiation Therapy (EBRT): Used palliatively to manage bone metastases and prevent complications such as spinal cord compression.
- Thermal Ablation: Both radiofrequency and microwave thermal ablation techniques are used to relieve pain and manage functional impairments.
What Are the Risk Factors for Medullary Thyroid Cancer?
The risk factors for medullary thyroid cancer are mostly genetic and linked to hereditary syndromes. Although environmental factors have also been studied, no clear results have been found. The most important risk factor for MTC is mutations in the RET proto-oncogene, which underlie both hereditary and sporadic cases.
Genetic Mutations:
- RET proto-oncogene mutations are the most common genetic cause of MTC.
- Specific RET mutations, such as M918T, are associated with a more aggressive disease course.
Hereditary Syndromes:
- MEN2A syndrome is characterized by medullary thyroid cancer, pheochromocytoma, and hyperparathyroidism.
- MEN2B syndrome is more aggressive and includes mucosal neuromas and marfanoid habitus.
- Familial Medullary Thyroid Carcinoma (FMTC) is a familial form of MTC.
Individuals carrying hereditary RET mutations are at increased risk of developing MTC at a younger age. Cases associated with MEN2A and MEN2B syndromes typically present earlier and are generally more aggressive.
Sporadic MTC: Sporadic MTC is non-hereditary and associated with somatic mutations in the RET gene developed during life. While environmental factors have not played a strong role in this form, some studies have suggested that radiation may have a minor effect.
T and N Staging: Tumor size and lymph node involvement are critical factors determining disease course. Patients with higher stages have a greater risk of recurrence and metastasis.
When Can Medullary Thyroid Cancer Treatment Be Performed?
In the treatment of medullary thyroid cancer, interventional radiology techniques are especially applied when the disease is localized or to alleviate symptoms in advanced stages. These techniques play an important role in the management of oligometastatic disease, where metastases are limited in number and specific regions. They are especially used for small metastatic lesions in the liver, bones, and lungs. Interventional radiology treatments are applied to control tumor growth and reduce symptoms caused by metastatic lesions.
The main interventional radiology techniques used in medullary thyroid cancer treatment are:
- Radiofrequency ablation (RFA): Controls tumor growth by targeting small metastatic lesions.
- Embolization: Used to reduce tumor burden and relieve symptoms in liver metastases.
- Cryoablation: Particularly effective for pain control and managing complications in bone metastases.
These treatments are preferred when surgery is not possible or carries high risk. RFA is especially effective in recurrent tumors or unresectable metastatic lesions. Additionally, embolization is effective in reducing tumor burden and symptoms, especially in liver metastases. Interventional radiology techniques also play an important role in managing complications such as spinal cord compression.
When Is Medullary Thyroid Cancer Treatment Not Possible?
Interventional radiology treatment may not always be possible in medullary thyroid cancer. The main reasons include tumor location, size, and the patient’s overall health status. The risks associated with specific interventional radiology methods must also be considered. These factors can decrease the likelihood of success and increase the risk of serious complications.
- Radiofrequency Ablation (RFA): This method is not preferred if the tumor is too close to the trachea, esophagus, or recurrent laryngeal nerve, as these vital structures are vulnerable to thermal injury during the procedure. Larger tumor sizes may also require more sessions and carry higher risk. If the patient has severe comorbidities or poor general condition, anesthesia may not be feasible.
- Ethanol Ablation: Not applicable when the tumor is near critical structures due to the risk of ethanol leakage damaging adjacent vital structures. Complete necrosis may not be possible in large or heterogeneous tumors, increasing the risk of recurrence.
- Laser Ablation: Not suitable if the tumor is close to important neck structures. Complex tumor shapes or large sizes pose a risk for precise targeting. Long ablation times may not be tolerated in patients with poor anesthesia tolerance.
What Is the Recovery Process After Medullary Thyroid Cancer Treatment?
The recovery process after medullary thyroid cancer treatment varies depending on the patient’s condition and the methods used. Interventional radiology treatments generally speed up postoperative recovery. After ablation techniques, patients typically recover quickly, often feeling better within a few days. Recovery is also effective after procedures such as cryoablation or thermal ablation, and most patients can return to daily activities within a week. For more complex procedures such as radioembolization, the recovery process may extend over several weeks.
Key points to monitor during recovery include:
- Monitor for pain and discomfort after the procedure.
- Be aware of infection or bleeding risk.
- Regular follow-up imaging is required for patients.
- Calcitonin and CEA levels should be monitored.
- Further treatment may be needed in case of tumor recurrence.
How Can Medullary Thyroid Cancer Be Prevented?
Prevention of medullary thyroid cancer focuses on genetic screening and early intervention for hereditary forms. Since hereditary cases make up a significant proportion of the disease, identifying individuals at risk is important. Early genetic testing plays a critical role for family members. For individuals with hereditary RET mutations, the following precautions are recommended:
- Early genetic screening
- Prophylactic thyroidectomy
- Regular monitoring of family members
Children with RET mutations should be evaluated at an early age for preventive purposes. In sporadic forms, early diagnosis is important. Monitoring calcitonin levels is recommended for individuals with thyroid nodules.
Genetic prevention is less applicable in sporadic cases, but early diagnosis by monitoring is possible. Early surgical intervention reduces the risk of metastasis. In advanced disease, targeted therapies should be considered.
Tyrosine kinase inhibitors such as vandetanib and cabozantinib are among the treatment options. These therapies aim to slow disease progression. In summary, genetic testing and surgical measures are crucial in hereditary cases. In sporadic cases, monitoring and early surgical intervention are of vital importance.
Frequently Asked Questions
What is the relationship of medullary thyroid cancer with genetic factors?
Medullary thyroid cancer (MTC) is significantly genetic, with about 25% of cases being hereditary. This is generally caused by germline mutations in the RET proto-oncogene and is associated with Multiple Endocrine Neoplasia Type 2 (MEN2) syndromes, particularly MEN2A and MEN2B. MEN2 syndromes are often accompanied by additional endocrine tumors such as pheochromocytoma and parathyroid adenomas. Seventy-five percent of MTC cases are sporadic, and 50% of these patients have somatic RET mutations. The most common somatic mutation, RET M918T, is seen in 80% of sporadic MTC cases. In 70% of RET-negative sporadic MTCs, RAS mutations are detected. Genetic testing for RET mutations in all MTC patients allows the identification of hereditary cases and early diagnosis and intervention for at-risk family members.
Which symptoms are more common in this cancer type?
Medullary thyroid cancer (MTC) usually appears as a painless lump or nodule in the neck related to the thyroid gland. As the disease progresses, symptoms such as neck pain, difficulty swallowing (dysphagia), difficulty breathing (dyspnea), and voice changes or hoarseness may occur if the nerves controlling the vocal cords are affected. Advanced MTC, due to increased calcitonin produced by the C cells of the thyroid, can result in symptoms such as diarrhea and facial flushing. In the United States, MTC accounts for about 1–2% of thyroid cancers, and 25% of these cases are hereditary, usually associated with Multiple Endocrine Neoplasia syndromes (MEN 2A and MEN 2B). Early diagnosis is important as MTC can spread to lymph nodes and other organs; early detection of these symptoms can significantly impact treatment outcomes.
How effective is surgical treatment in medullary thyroid cancer?
Surgical treatment is the most effective and curative approach in medullary thyroid cancer (MTC); the standard procedure is total thyroidectomy. However, for early-stage, localized MTC (T1 tumors), less extensive surgeries, such as lobectomy or subtotal thyroidectomy, provide similar long-term survival outcomes. A population analysis showed no significant difference in cancer-specific mortality rates between total and limited thyroidectomy in T1N0/1M0 MTC patients. Achieving a biochemical cure, shown by undetectable serum calcitonin levels after surgery, increases survival rates. Lymph node involvement and the metastatic lymph node ratio are important prognostic factors for both biochemical cure and disease-specific survival. Therefore, although surgical intervention is the cornerstone of MTC treatment, the extent of surgery should be individualized according to tumor stage and patient factors.
How are calcitonin levels monitored during treatment?
During the treatment of medullary thyroid cancer (MTC), calcitonin levels are regularly monitored by blood tests to assess disease status and detect recurrence. Achieving undetectable calcitonin levels after surgical removal of the thyroid indicates a favorable outcome. High or rising calcitonin levels suggest persistent or recurrent disease and require further evaluation. The doubling time of calcitonin levels is an important prognostic factor; a period shorter than two years is associated with a poorer prognosis. In some cases, when basal levels are inconclusive, stimulation tests using agents such as calcium or pentagastrin may be performed to detect residual disease. Regular monitoring of calcitonin levels, together with imaging studies, is necessary for effective management of MTC.
What complications may occur if medullary thyroid cancer is not diagnosed early?
If Medullary Thyroid Cancer (MTC) is not diagnosed early, about 70% of patients have cervical metastases when thyroid nodules become palpable, and 10% are diagnosed with distant metastases. In high-grade MTC patients, the mortality rate is 45.4%, while in low-grade cases, this rate is 2.1%; only 9.1% of high-grade patients remain cancer-free, compared to 70.5% of low-grade patients. Surgery performed more than one month after diagnosis negatively affects overall survival rates. These data show that early diagnosis and rapid treatment are critical for improving survival rates in MTC.

Girişimsel Radyoloji ve Nöroradyoloji Uzmanı Prof. Dr. Özgür Kılıçkesmez, 1997 yılında Cerrahpaşa Tıp Fakültesi’nden mezun oldu. Uzmanlık eğitimini İstanbul Eğitim ve Araştırma Hastanesi’nde tamamladı. Londra’da girişimsel radyoloji ve onkoloji alanında eğitim aldı. İstanbul Çam ve Sakura Şehir Hastanesi’nde girişimsel radyoloji bölümünü kurdu ve 2020 yılında profesör oldu. Çok sayıda uluslararası ödül ve sertifikaya sahip olan Kılıçkesmez’in 150’den fazla bilimsel yayını bulunmakta ve 1500’den fazla atıf almıştır. Halen Medicana Ataköy Hastanesi’nde görev yapmaktadır.







Vaka Örnekleri