Vasoconstriction is the narrowing of blood vessels caused by contraction of the muscular wall of arteries. This physiological response regulates blood pressure and redirects circulation during stress or cold exposure.
Pathological vasoconstriction may contribute to hypertension, migraines, and peripheral artery disease. It can impair blood flow and increase cardiovascular risks if persistent.
Pharmacological agents that induce vasoconstriction include decongestants, certain anesthetics, and vasopressors. These medications are used in clinical settings to control bleeding or maintain blood pressure.
Treatment of excessive vasoconstriction focuses on vasodilator medications, lifestyle adjustments, and addressing underlying conditions to restore proper vascular function.
| Definition | An increase in intravascular pressure due to the narrowing of blood vessels. It is usually triggered by the sympathetic nervous system or certain chemical substances. |
| Physiological Mechanism | The diameter of the vessel decreases as the smooth muscles in the vessel wall contract, which reduces blood flow and increases blood pressure. |
| Causes | Cold weather, stress, pain, certain medications (adrenaline, noradrenaline, vasopressor agents), substances like smoking and caffeine, hormonal changes. |
| Effects | Increase in blood pressure, decrease in blood flow, reduced oxygen delivery to tissues, organ damage in some cases. |
| Relationship to Pathological Conditions | It plays an important role in hypertension, Raynaud’s disease, migraine, cardiovascular diseases, shock, and organ failure. |
| Triggering Substances | Hormones: Adrenaline, noradrenaline, vasopressin, angiotensin II. Medications: Decongestants (pseudoephedrine), vasopressor agents, some migraine medications (triptans). |
| Treatment and Management | Vasodilator drugs (nitrates, calcium channel blockers), heat application, stress management, reduction of smoking and caffeine consumption. |
What is Vasoconstriction?
Vasoconstriction means the reduction in the diameter of blood vessels due to the contraction of smooth muscles surrounding the blood vessels. With the narrowing of the vessels, the speed and pressure of the blood flow change. The dilation (vasodilation) and narrowing (vasoconstriction) of vessels in the body are primarily controlled by the autonomic nervous system as a delicate balance. By maintaining this balance, your body ensures that tissues are adequately nourished and can rapidly regulate blood pressure when necessary.
At the heart of this mechanism is usually the sympathetic nervous system. When sympathetic stimulation increases, released norepinephrine (also known as noradrenaline) and similar chemical messengers bind to alpha-1 and alpha-2 adrenergic receptors on smooth muscle cells in the vessel wall. This raises the intracellular calcium level. Increased calcium causes the contractile proteins (actin-myosin) to slide over each other, resulting in the contraction of the vessel muscle and narrowing of the vessel lumen. This narrowing creates increased resistance to blood flow. To visualize this, imagine squeezing the end of a garden hose to make the water spray more forcefully.
In our bodies, vasoconstriction is not only triggered by neural stimulation; various chemicals can also initiate this process. For example, endothelin secreted by the vascular endothelium, thromboxane produced by platelets, and certain hormonal systems (such as the renin-angiotensin system) have vasoconstrictor effects. Additionally, external factors such as cold weather can cause peripheral (surface) vessels to constrict to minimize heat loss.
What Are the Causes of Vasoconstriction?
The factors triggering vasoconstriction are quite diverse. These can be grouped under physiological (normal body function), environmental, and pathological (disease-related) headings.
- Cold Exposure: The main reason your hands and feet feel colder when you’re cold is decreased blood flow to the skin. The body constricts small vessels in the skin to minimize heat loss, protecting vital internal organs as a defense mechanism.
- Stress and Sympathetic Activation: In stressful moments, known as the “fight or flight” response, the sympathetic nervous system becomes active. Released norepinephrine and epinephrine constrict vessels and raise blood pressure. This prepares the body for emergencies: the brain and muscles get enough blood, while less urgent systems like digestion receive less flow.
- Smoking and Other Chemicals: Nicotine and other toxic substances in cigarette smoke directly cause contraction of the smooth muscles in vessel walls. This can contribute to chronic high blood pressure over time. Similarly, excessive caffeine intake can also cause some degree of vessel constriction.
- Hormonal and Biochemical Factors: Substances such as serotonin, endothelin-1 (ET-1), angiotensin II (ANG II), histamine, and prostaglandins also play a role in determining vessel tone. Endothelin-1 is one of the strongest known vasoconstrictors. Angiotensin II is key for the kidneys’ blood pressure regulation.
- Psychological or Mental Stress: Some studies show that intense mental activity or emotional stress can cause vessel constriction, especially in visceral organs. This effect may be more pronounced in individuals with poor stress management.
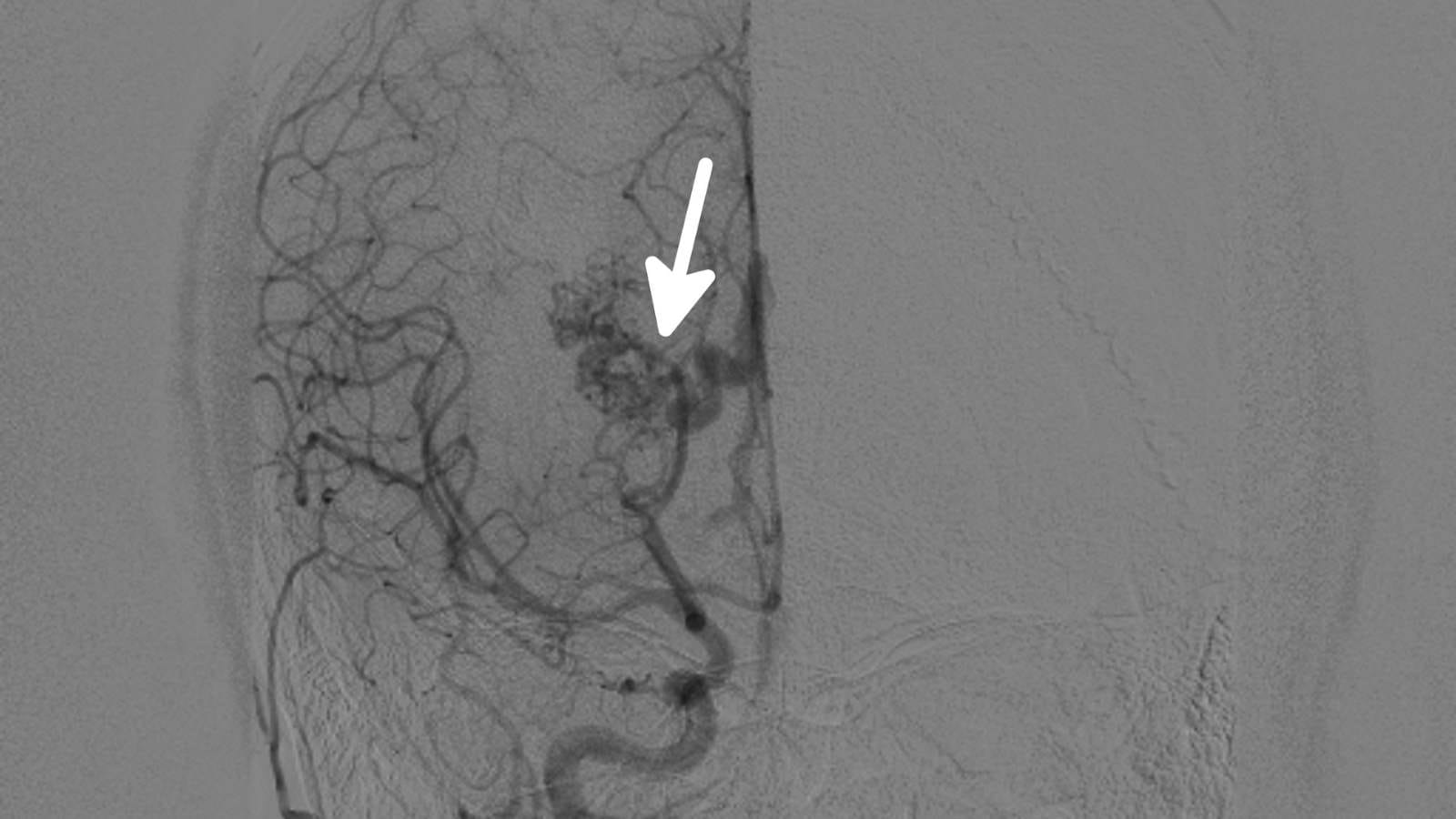
- Medical Conditions and Diseases: In diseases like Raynaud’s phenomenon, exposure to cold or stress causes excessive constriction in the fingers’ vessels, resulting in pain, blanching, or even discoloration. Certain brain conditions (such as subarachnoid hemorrhage) can also cause temporary or permanent constriction of cerebral vessels.
- Medications: Many medications exert therapeutic effects by increasing vasoconstriction in target tissues. For example, pseudoephedrine commonly used in nasal sprays narrows the vessels in the nasal passages, easing congestion.
How Does Vasoconstriction Regulate Blood Flow?
Blood flow is closely related to changes in vessel diameter. When a vessel narrows, the speed and pressure of the blood flowing through it change. This can be explained by Poiseuille’s law: resistance is inversely proportional to the fourth power of the vessel’s radius. In practice, even a small narrowing significantly increases vascular resistance.
- Relationship Between Resistance and Blood Pressure: When vessels narrow, the heart must produce a higher pressure to pump the same amount of blood. This naturally raises systemic blood pressure. The body maintains blood pressure within a certain range this way. For example, when you stand up quickly, vessels constrict rapidly to ensure enough blood reaches the brain and prevent dizziness.
- Redistribution of Blood: The body adjusts blood flow to different regions as needed. For example, during intense exercise, blood vessels to skeletal muscles dilate while digestive tract vessels constrict. This prioritizes oxygen and nutrients for muscles and shifts digestion to the background.
- Organ Perfusion: Through a mechanism called autoregulation, organs such as the brain and kidneys adjust their vessels to maintain ideal pressure and flow. Vasoconstriction can reduce blood flow in certain areas and direct it to other regions, helping protect vital organs. For example, during severe blood loss, vessels in the leg muscles constrict to redirect blood to the brain and heart.
- Sympathetic Nervous System and Local Factors: Smooth muscles in vessel walls are highly sensitive to both neural and local chemical stimuli. Global sympathetic activation during stress can cause simultaneous vasoconstriction in multiple regions, while locally secreted substances in damaged or inflamed tissue may have region-specific vasoconstrictor or vasodilator effects.
What Role Does Vasoconstriction Play in Maintaining Body Temperature?
The body works hard to maintain heat balance. One of the most obvious examples is how quickly our hands and feet get cold in winter. When exposed to cold, the body constricts the vessels under the skin. The purpose of this narrowing is to reduce heat loss by limiting blood flow to the skin and prioritize circulation in vital organs.
- Reducing Heat Loss at the Skin: When superficial vessels constrict, less blood reaches the skin, lowering skin temperature and minimizing heat loss to the environment. Cold exposure causing the ears, nose, hands, and feet to feel cold is normal for this reason.
- Central Heat Conservation: Maintaining core temperature is critical for the optimal functioning of organs like the brain and heart. Constriction of peripheral vessels helps trap heat in the core, acting as a defense line against hypothermia.
- Thermoregulation Mechanisms: The hypothalamus in the brain acts as the “body’s thermostat,” sending commands based on signals from skin temperature receptors. When temperature drops, the shivering reflex is activated, metabolism increases, and vessels constrict. This increases heat production and reduces heat loss to the environment.
Imagine going for a run on a cold day. At first, your hands get cold, but as your body warms up, your blood vessels dilate, and your fingers warm up. After you finish running and your body starts to cool down, vessel constriction returns. All these fluctuations are controlled unconsciously by the autonomic nervous system.
Can Vasoconstriction Be Beneficial for Certain Medical Conditions?
Although vasoconstriction may sound negative as “narrowing of the vessels,” in some medical situations it is actually beneficial. Here are some examples of its positive effects:
- Bleeding Control: During injury or surgery, the body automatically constricts vessels to reduce blood loss as a natural defense. Local vasoconstrictor medications (such as solutions containing epinephrine) are also used to minimize bleeding during surgery.
- Shock Treatment: In emergencies such as hypotension (low blood pressure) or anaphylactic shock, vasoconstrictor (vasopressor) medications are given to quickly raise blood pressure and ensure sufficient blood flow to vital organs.
- Migraine Relief: Some migraines are associated with dilation of certain blood vessels. Caffeine or migraine medications (such as triptans) can relieve pain by constricting these dilated vessels.
- Local Anesthetic Applications: In dental treatments or minor surgery, epinephrine is sometimes added to local anesthetic solutions. This constricts vessels at the injection site, slows the spread and removal of the drug, and prolongs the effect of the anesthesia.
- Temperature Regulation and Raynaud-like Conditions: In Raynaud’s phenomenon, conscious and controlled temperature management or short-term “therapeutic” vasoconstriction can be used to regulate circulation. In mild or temporary cases, vessel tone can be optimized with controlled exposure to cold/heat or medications.
What Are the Potential Risks and Side Effects of Excessive Vasoconstriction?
Like anything excessive, excessive or uncontrolled vasoconstriction can lead to various problems. These risks can be grouped as follows:
- High Blood Pressure (Hypertension): If vessels remain constricted, the heart must generate greater pressure to supply the body’s needs. Chronic high blood pressure can develop over time, increasing the risk of heart attack, stroke, and other serious complications.
- Tissue and Organ Ischemia: Severely constricted vessels may not deliver enough oxygen and nutrients to tissues. Prolonged constriction can cause cell damage or cell death. For example, in Raynaud’s phenomenon, the fingertips turn white and cold; in advanced cases, severe pain and even tissue loss can occur.
- Negative Effects on the Heart: Persistently high vascular resistance strains the heart’s pumping function. This can lead to structural changes in the heart muscle (thickening of the heart wall) and increase the risk of heart failure.
- Cerebral Vasoconstriction and Headaches: In conditions like Reversible Cerebral Vasoconstriction Syndrome (RCVS), severe narrowing of brain vessels can cause sudden, severe headaches and increase the risk of stroke.
- Problems with Heat Regulation: Chronic or excessive vasoconstriction can prevent the body from dissipating heat. If vessels can’t dilate sufficiently in hot environments, serious problems such as heat stroke can occur.
- Drug Side Effects: Uncontrolled use of vasoconstrictor medications (such as prolonged use of nasal sprays) can cause a “rebound” effect, where the vessels dilate excessively when the medication is stopped, leading to more severe symptoms.
How Are Drugs Used to Treat Certain Health Conditions with Vasoconstriction?
Drugs with vasoconstrictive effects are used in many fields of medicine. These drugs can regulate blood flow in a specific area, reduce tissue swelling, or increase systemic blood pressure by causing vessel constriction.
- Decongestants (Nasal Sprays, Tablets): In upper respiratory infections, nasal congestion occurs as vessels in the nasal mucosa dilate and swell. Decongestants (such as pseudoephedrine, phenylephrine) constrict these vessels, reducing swelling and congestion, and making it easier to breathe. However, overuse can cause damage to the nasal mucosa or conditions such as “rebound rhinitis.”
- Treatment of Hypotension and Shock: In emergency settings, vasopressors such as intravenous norepinephrine, dopamine, or epinephrine are administered to patients in anaphylactic or septic shock to quickly raise blood pressure. These drugs cause vessel constriction throughout the vascular system, ensuring continued blood flow to tissues. If blood pressure remains too low, vital organs such as the brain and heart are at risk, so these drugs are life-saving.
- Bleeding Control in Surgery: Adding epinephrine to local anesthetic solutions constricts vessels in the area, prolongs the effect of anesthesia, and minimizes bleeding. This method is frequently used in dentistry or skin incision operations.
- Eye Drops: In some eye diseases (such as glaucoma), changes in vascular pressure are important. In selected cases, drops with vasoconstrictive effects can be used to regulate intraocular pressure.
- Dopamine and Other Cardiovascular Drugs: Dopamine dilates kidney vessels at low doses, but at moderate to high doses, its vasoconstrictive effect increases blood pressure. In intensive care settings, doctors carefully adjust the dose to achieve optimal blood pressure and organ perfusion based on the patient’s condition.
- Hormonal System Regulators: The opposite effect of angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARB) is vasodilation, lowering blood pressure. However, hormones like vasopressin (ADH) can cause vessel constriction when needed. This balance is managed through medication choice and dose adjustment.
What Is the Relationship Between Vasoconstriction and Vascular Resistance?
One of the main results of vasoconstriction is increased vascular resistance. The narrower the vessel, the greater the friction and pressure the blood encounters. To understand this, think of this analogy: when you squeeze a thick hose with a narrow tip, the flow of water becomes faster, but the pressure inside the hose also increases.
- Systemic Vascular Resistance (SVR): Large vessels, especially arteries, are the main routes for pumping blood. Narrowing of these arteries creates more resistance in front of the heart. The heart can overcome this resistance, but the result is increased blood pressure.
- Effect of Chronic Vasoconstriction: If vasoconstriction is long-term (due to stressful life, high salt intake, or genetic predisposition), vessel walls may thicken and lose elasticity, leading to chronic high blood pressure.
- Myogenic Mechanism and Cellular Changes: Smooth muscle cells in vessel walls can contract in response to increased pressure on the inner wall. This reflex (myogenic response) stabilizes blood flow at the level of small arteries. However, when excessive or frequently repeated, it can cause structural changes in the vessel.
- Venous Return and Cardiac Output: Arterial vasoconstriction creates resistance in blood leaving the heart; venous constriction affects the amount of blood returning to the heart. Narrowing at both ends directly affects the efficiency of the heart. If veins constrict, less blood returns to the heart, and cardiac output may fall.
How Does Vasoconstriction Contribute to Cold Responses?
One of the first responses when we are exposed to cold is the constriction of skin blood vessels. This process can be explained by several mechanisms:
- Sympathetic Activation: When cold air stimulates skin receptors, the brain sends a “constrict” signal to peripheral vessels via the sympathetic nervous system. Blood flow to the extremities (hands, feet, ears) decreases, minimizing heat loss.
- Rho Kinase and Other Enzymes: Research shows that cold activates certain enzymes (such as Rho kinase) in the vessel wall, increasing smooth muscle contraction. This biochemical pathway is a key mechanism for heat conservation.
- TRP Channels: Cold-sensing channels in our skin (especially TRPA1) are sensitive to cold. When exposed, they increase intracellular calcium, triggering contraction. This produces a rapid and localized vasoconstriction.
- Adaptation to Thermal Gradients: The body creates a layered “thermal barrier” to retain heat. If the outside air is very cold, skin vessels constrict, restricting blood flow and strengthening this “thermal insulation layer.” Of course, with prolonged and severe cold, the risk of frostbite emerges, so this mechanism is not unlimited.
- Behavioral Responses: Reflexes such as putting your hands in your pocket or warming them with your breath support this physiological narrowing. Hands and feet are the areas most susceptible to heat loss, so the body automatically limits blood flow to these regions for protection.

Girişimsel Radyoloji ve Nöroradyoloji Uzmanı Prof. Dr. Özgür Kılıçkesmez, 1997 yılında Cerrahpaşa Tıp Fakültesi’nden mezun oldu. Uzmanlık eğitimini İstanbul Eğitim ve Araştırma Hastanesi’nde tamamladı. Londra’da girişimsel radyoloji ve onkoloji alanında eğitim aldı. İstanbul Çam ve Sakura Şehir Hastanesi’nde girişimsel radyoloji bölümünü kurdu ve 2020 yılında profesör oldu. Çok sayıda uluslararası ödül ve sertifikaya sahip olan Kılıçkesmez’in 150’den fazla bilimsel yayını bulunmakta ve 1500’den fazla atıf almıştır. Halen Medicana Ataköy Hastanesi’nde görev yapmaktadır.







Vaka Örnekleri