A saccular aneurysm is a balloon-like bulge on one side of a blood vessel wall, commonly seen in brain arteries. It carries a high risk of rupture, leading to life-threatening bleeding.
Symptoms may include sudden severe headache, vision problems, or neurological deficits. Many cases remain silent until rupture occurs, highlighting the importance of early detection.
Diagnosis relies on imaging techniques such as CT angiography, MRI, or digital subtraction angiography, which provide detailed vessel visualization.
Treatment options include surgical clipping or endovascular methods such as coiling and stent placement. Both approaches aim to prevent rupture and secure long-term vascular stability.
| Disease Name | Saccular Aneurysm |
| Definition | A type of aneurysm with a pouch-like structure forming as a ballooning of brain vessels, especially seen at vessel bifurcation points. |
| Symptoms | Small aneurysms are usually asymptomatic; large or ruptured aneurysms may cause symptoms such as headache, visual disturbances, facial pain, double vision, nausea, vomiting, and loss of consciousness. |
| Causes | Genetic predisposition, hypertension, smoking, congenital weakness in vessels, head trauma, some infections, and diseases affecting vessel structure. |
| Risk Factors | Family history of aneurysm, hypertension, smoking and alcohol use, advanced age, female sex, polycystic kidney disease, and certain connective tissue disorders. |
| Diagnostic Methods | Brain CT angiography, MR angiography, digital subtraction angiography (DSA – gold standard), brain MRI (to evaluate brain tissue after bleeding). |
| Treatment Methods | Observation for small and asymptomatic aneurysms; endovascular coiling, surgical clipping, or flow diverter stent placement for symptomatic or high-risk aneurysms. |
| Complications | Subarachnoid hemorrhage due to aneurysm rupture, brain tissue damage, stroke, permanent neurological deficits, high mortality risk. |
| Follow-up and Monitoring | Small and asymptomatic aneurysms are monitored with regular imaging; routine check-ups are performed after treatment to prevent recurrence. |
| Prevention Methods | Blood pressure control, avoiding smoking, limiting alcohol consumption, healthy diet, stress management; regular imaging for high-risk individuals. |
| Associated Diseases | Subarachnoid hemorrhage, stroke, connective tissue diseases (e.g., Ehlers-Danlos syndrome), polycystic kidney disease. |
Prof. Dr. Özgür KILIÇKESMEZ Prof. Dr. Kılıçkesmez holds the Turkish Radiology Competency Certificate, the Turkish Interventional Radiology Competency Certificate, Stroke Treatment Certification, and the European Board of Interventional Radiology (EBIR). In his academic career, he won the Siemens Radiology First Prize in 2008.
Interventional Radiology / Interventional Neuroradiology
What Is a Saccular Aneurysm?
A saccular aneurysm, also known as a “berry” aneurysm, is a round, pouch-like protrusion of a vessel. It typically develops at arterial branching points in the brain, especially in regions with high hemodynamic stress. It is frequently observed in the circle of Willis, which is crucial for cerebral blood flow. Saccular aneurysms constitute the majority of intracranial aneurysms and, due to weakened vessel walls, carry a risk of rupture. In the event of rupture, they cause subarachnoid hemorrhage, a life-threatening condition. It is associated with high morbidity and mortality rates. Hypertension, smoking, and genetic factors are among the main risk factors for saccular aneurysm formation.
What Are the Causes of Saccular Aneurysm?
Many factors play a role in the formation of saccular aneurysm, and these interact with each other. First, hemodynamic stress has a significant effect at arterial bifurcation points, where intravascular pressure rises. These sites are exposed to high wall shear stress and turbulent blood flow, making endothelial damage inevitable. This triggers changes in the vessel wall, creating a basis for aneurysm formation.
Chronic inflammation processes also play an important role. These processes are characterized by the secretion of cytokines and inflammatory mediators by immune cells. These cells weaken the smooth muscle cells and extracellular matrix that support the vessel wall. Inflammatory responses remodel the vessel wall and facilitate aneurysm development.
- Genetic and familial factors: Genetic predisposition is among the key causes of saccular aneurysm. Mutations in certain genes compromise vessel integrity and increase susceptibility to aneurysms. Family history also increases these risks.
- Atherosclerosis: Lipid accumulation and infiltration of inflammatory cells into the vessel wall reduce the structural support of elastic tissue, promoting aneurysm development.
*We recommend filling out all fields so we can respond in the best possible way.
How Common Is Saccular Aneurysm?
The prevalence of saccular aneurysms in the general population varies between 2% and 5%. These rates may vary depending on geographic and demographic factors. Saccular aneurysms are more common in women, with a male-to-female ratio of 1:2. They are frequently seen in individuals over the age of 50, with the highest incidence in the 50-60 age range. Geographically, the incidence of subarachnoid hemorrhage is high in Finland and Japan.
Demographic factors also play an important role, as saccular aneurysms are more common in individuals with certain risk factors. Main risk factors include:
- Hypertension
- History of smoking
- Family history of aneurysm
Certain connective tissue disorders also increase the risk of aneurysm. Diseases such as autosomal dominant polycystic kidney disease and Marfan syndrome are considered high risk. About 20-30% of patients have more than one aneurysm, indicating that some individuals may develop multiple aneurysms over time.
Anatomically, saccular aneurysms generally occur at bifurcation points in the circle of Willis. The most common locations are:
- Anterior communicating artery (30-35%)
- Internal carotid artery (30%)
- Middle cerebral artery (22%)
The risk of aneurysm rupture is directly proportional to the size of the aneurysm, especially if the diameter exceeds 7 mm. While rupture risk is low, it remains an important factor.
What Is the Formation Process of Saccular Aneurysm?
The formation process of saccular aneurysms begins with the interaction of many hemodynamic, structural, and biological factors. These aneurysms are generally found at arterial bifurcation sites in the circle of Willis, as these regions are exposed to high wall shear stress and localized pressure. This leads to dysfunction of endothelial cells and initiates remodeling of the vessel wall. In the early stages, the inner elastic lamina and smooth muscle layer of the artery wall are damaged.
This damage disrupts the integrity of the vessel wall and facilitates the migration of inflammatory cells into the wall. Inflammatory cells secrete enzymes and cytokines that contribute to weakening of the vessel wall. During this process, degradation of the extracellular matrix and thinning of the wall also occur. The weakened arterial wall undergoes marked structural changes, creating a basis for aneurysm formation. These structural changes include intimal hyperplasia and irregularities in vascular smooth muscle cells.
- Chronic inflammation plays a major role in the later stages of the process.
- This inflammatory response causes a decrease in elastin and an increase in collagen in the vessel wall.
- Vascular remodeling leads to decreased resistance against hemodynamic forces.
In advanced stages, atherosclerotic changes occur in the arterial wall, with increased infiltration of lipid-laden macrophages. This further weakens the structure of the vessel wall. Persistent hemodynamic stress such as high blood pressure and turbulent blood flow increases the risk of rupture. Ongoing stress maintains endothelial damage and triggers inflammation, resulting in thinning of the vessel wall.
What Are the Symptoms of Saccular Aneurysm?
The symptoms of saccular aneurysms differ depending on whether or not they have ruptured. Unruptured aneurysms are usually asymptomatic but may cause symptoms if they grow large enough to compress brain tissues. In such cases, common symptoms include:
- Headaches
- Visual changes, blurred or double vision
- Eye pain
- Pupil dilation
Some patients may experience facial numbness and weakness or drooping of the eyelid. However, if a saccular aneurysm ruptures, it leads to subarachnoid hemorrhage, causing sudden and severe symptoms. The most prominent symptom is an intense headache. Additionally, nausea, vomiting, neck stiffness, and photophobia may be seen. Seizures, confusion, or loss of consciousness can also occur. Sometimes, warning headaches may develop before rupture.
How Is Saccular Aneurysm Diagnosed?
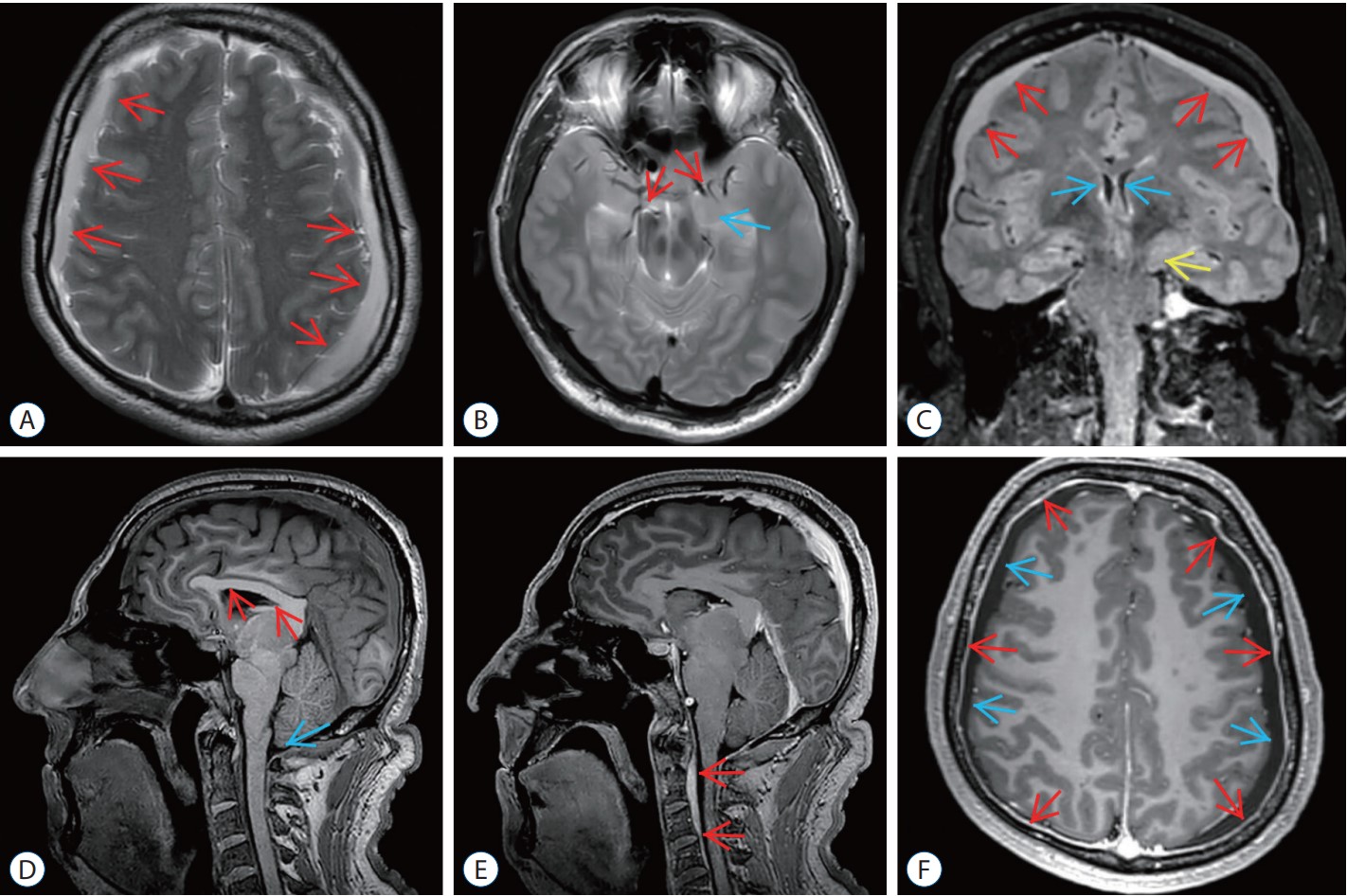
The diagnosis of saccular aneurysms is generally made using various imaging techniques. The most commonly used methods for accurate detection of intracranial aneurysms are Computed Tomography Angiography (CTA), Magnetic Resonance Angiography (MRA), and Digital Subtraction Angiography (DSA). Each of these methods offers different advantages in the diagnostic process.
- CTA and MRA: These are known as non-invasive techniques and cause less discomfort to the patient. CTA in particular provides a detailed view of the cerebral vascular system and high-resolution three-dimensional images of aneurysms. MRA allows for detailed vessel imaging without radiation exposure.
- DSA: DSA is a more invasive technique than the others. However, it is accepted as the “gold standard” for definitive aneurysm imaging. This method is especially useful for evaluating complex cases and helps with surgical planning.
How Is Saccular Aneurysm Treated?
The treatment of saccular aneurysms is performed with minimally invasive methods and aims to reduce blood flow and prevent the risk of aneurysm rupture. Endovascular methods are prominent among the main techniques used. These methods are selected based on the size, location, and structure of the aneurysm and are tailored to the patient.
Main treatment techniques include:
- Coiling: This method is frequently used for small aneurysms and blocks the vessels by forming thrombosis within the aneurysm. Platinum coils are placed inside the aneurysm and are especially effective for those without a wide neck.
- Stent-Assisted Coiling (SAC): The SAC method is used to prevent coil migration in wide-necked aneurysms. SAC provides structural support at arterial bifurcations. However, since it requires dual antiplatelet therapy (DAPT), it is preferred in unruptured aneurysms.
- Flow Diversion: This technique is highly effective for wide-necked aneurysms and those in hard-to-reach locations. It directs blood flow to provide occlusion and has a relatively low complication rate. However, it also requires DAPT, limiting its use to unruptured cases.
- Woven EndoBridge (WEB) Device: The WEB device is a method developed for wide-necked bifurcation aneurysms. It disrupts blood flow to create thrombosis and does not require DAPT, making it suitable for both ruptured and unruptured aneurysms.
What Are the Complications of Saccular Aneurysm?
The complications of saccular aneurysm can have serious consequences and greatly affect the patient’s quality of life. The most common complication after rupture is subarachnoid hemorrhage (SAH), which can lead to death or permanent neurological damage. Especially after rupture, lack of oxygen in brain tissue causes ischemic injury. These complications are related to the size and location of the aneurysm as well as the general health of the patient.
Other complications include cerebral vasospasm, hydrocephalus, and encephalopathy. After rupture, blood spreading over the brain surface leads to vasospasm, which restricts cerebral blood flow and creates additional ischemic damage. Cerebral vasospasm generally occurs within the first week after rupture and can cause severe neurological symptoms such as loss of consciousness. Hydrocephalus develops when blood blocks the circulation of cerebrospinal fluid, increasing intracranial pressure.
Additional complications of saccular aneurysm include:
- Neurological deficits: Long-term cognitive and motor function loss may occur.
- Epilepsy: Recurrent seizures may develop after aneurysm rupture.
- Loss of vascular integrity: Weakening and further dilation of blood vessel walls may continue.
- Increased intracranial pressure: Especially in association with hydrocephalus, increased pressure may further damage the brain.
What Is the Recovery Process After Saccular Aneurysm Treatment?
The recovery process after saccular aneurysm treatment varies depending on the method applied and the general health status of the patient. Recovery is usually faster after coiling and stent-assisted coiling (SAC) procedures. Patients are often monitored in intensive care and, if there are no complications, can be discharged shortly. During the first week at home, it is recommended to be careful and avoid strenuous activities.
As part of follow-up care:
- Imaging is performed at the 6th month and then annually or less frequently to assess aneurysm closure.
- Patients undergoing SAC for wide-necked aneurysms may require dual antiplatelet therapy.
The flow diversion method is preferred for complex aneurysms and has a slightly longer recovery period. In this method, antiplatelet therapy may be used for up to 6 months to reduce the risk of clotting. Typically during recovery:
- Angiographic evaluations are performed at 6 and 12 months.
- Close follow-up is required for bleeding and clotting risks after treatment.
Patients treated with the WEB device have a shorter recovery period. This minimally invasive method is suitable for wide-necked bifurcation aneurysms and generally does not require antiplatelet therapy. Patients can be discharged 1-2 days after the procedure. For these patients:
- Imaging follow-up is performed at 3 and 6 months to assess aneurysm occlusion.
- The long-term risk of complications is low, but regular check-ups are important.
How Can Saccular Aneurysm Be Prevented?
Various precautions should be taken to prevent saccular aneurysm. First, lifestyle changes are very important, as quitting smoking and maintaining a healthy lifestyle help protect vascular health. Smoking increases the risk of aneurysm by contributing to vascular inflammation. Blood pressure control is also essential, as high blood pressure increases both the risk of aneurysm development and rupture. Therefore, regular blood pressure monitoring and medication, if necessary, are recommended. Cholesterol management is also of great importance, as high cholesterol can damage vessel walls and trigger aneurysm formation by leading to atherosclerosis.
Anti-inflammatory therapies and antihypertensive drugs may be used as part of medical management, as these drugs help protect vascular health.
- Anti-inflammatory drugs may slow aneurysm progression by reducing inflammation in the vessel wall.
- Antihypertensive drugs balance blood pressure, reduce hemodynamic stress, and prevent vascular deterioration.
In addition, regular screening and surveillance are important, as they enable early diagnosis, especially in individuals with a family history of aneurysm.
- Imaging techniques can be used to monitor known aneurysms.
- Rupture risk can be assessed using risk scoring systems such as the PHASES score, and patient management can be planned accordingly.
Frequently Asked Questions
How does a saccular aneurysm form?
Saccular aneurysms, also called berry aneurysms, develop as a result of a combination of hemodynamic stress, structural defects in the vessel wall, and inflammatory processes. High shear stress and pressure from blood flow, especially at branching or curved regions of arteries, damage the inner elastic lamina and weaken the vessel wall. This weakening is exacerbated by inflammatory responses involving macrophages and lymphocytes, leading to remodeling of the vessel wall. Risk factors such as hypertension, smoking, and genetic predisposition increase the likelihood of developing saccular aneurysm.
How is the risk of aneurysm rupture assessed?
The risk of saccular aneurysm rupture is determined by evaluating the aneurysm’s size, location, patient demographics, and lifestyle habits. Approximately 51% of ruptured intracranial aneurysms are smaller than 7 mm. Aneurysms in the anterior communicating artery and other small intracranial arteries make up 35% and 14% of small ruptured aneurysms, respectively. Patients over 50 years of age, female sex, and a history of smoking are associated with higher rates of aneurysm growth. The annual rupture rate is 3.1% for growing aneurysms and 0.1% for stable ones. Additionally, non-saccular-shaped aneurysms have higher growth rates, indicating increased rupture risk. Hypertension and excessive alcohol consumption are also contributing factors. Evaluating these factors together helps determine the probability of aneurysm rupture and plan appropriate treatment strategies.

Girişimsel Radyoloji ve Nöroradyoloji Uzmanı Prof. Dr. Özgür Kılıçkesmez, 1997 yılında Cerrahpaşa Tıp Fakültesi’nden mezun oldu. Uzmanlık eğitimini İstanbul Eğitim ve Araştırma Hastanesi’nde tamamladı. Londra’da girişimsel radyoloji ve onkoloji alanında eğitim aldı. İstanbul Çam ve Sakura Şehir Hastanesi’nde girişimsel radyoloji bölümünü kurdu ve 2020 yılında profesör oldu. Çok sayıda uluslararası ödül ve sertifikaya sahip olan Kılıçkesmez’in 150’den fazla bilimsel yayını bulunmakta ve 1500’den fazla atıf almıştır. Halen Medicana Ataköy Hastanesi’nde görev yapmaktadır.







Vaka Örnekleri