Hepatomegaly refers to an enlarged liver, which may result from infections, metabolic disorders, heart failure, or liver diseases. It is a sign of an underlying condition rather than a disease itself.
Clinical evaluation includes physical examination, blood tests, and imaging methods such as ultrasound or MRI. These help determine the cause and extent of liver enlargement.
Common causes include fatty liver disease, viral hepatitis, alcohol-related damage, and congestive heart failure. Identifying the underlying pathology is crucial for proper treatment.
Management focuses on treating the primary cause, lifestyle modification, and in some cases, medication. Early diagnosis improves outcomes and prevents progression to liver failure.
| Definition | – Hepatomegaly is the condition where the liver is larger than normal. This enlargement can be due to a disease within the liver itself or another systemic problem. |
| Symptoms | – Feeling of fullness or pressure in the upper right abdomen – Abdominal pain (usually in the upper right quadrant) – Fatigue – Jaundice (yellowing of the skin and eyes) – Nausea, vomiting – Loss of appetite – Bloating or abdominal fluid accumulation (ascites) |
| Causes | Liver-Related: – Alcoholic liver disease – Non-alcoholic fatty liver disease (NAFLD) – Hepatitis (viral, toxic, or autoimmune) – Liver cirrhosis – Liver tumors (benign or malignant)Other Causes: – Heart failure (congestive hepatomegaly) – Blood diseases such as leukemia, lymphoma – Infections (e.g., malaria, mononucleosis) – Metabolic diseases (e.g., Wilson’s disease, hemochromatosis) |
| Risk Factors | – Excessive alcohol consumption – Obesity and metabolic syndrome – Viral infections (especially hepatitis B and C) – Family history of liver disease – Exposure to toxic substances |
| Diagnostic Methods | – Physical examination (liver palpation and percussion) – Blood tests (liver function tests, complete blood count) – Ultrasonography – Computed tomography (CT) or magnetic resonance imaging (MRI) – Liver biopsy (in necessary cases) |
| Treatment Options | – Treatment of the underlying cause: – Antiviral drugs for viral hepatitis – Diet and exercise for fatty liver disease – Cessation of alcohol for alcoholic liver disease – Supportive treatment: – Medication (anti-inflammatory, diuretics, etc.) – Surgery if necessary (e.g., tumor removal) |
| Complications | – Cirrhosis – Liver failure – Portal hypertension – Liver cancer (increased risk especially with cirrhosis) |
| Prevention | – Adopting a healthy and balanced diet – Avoiding excessive alcohol consumption – Protection against hepatitis B and C (vaccination and hygiene measures) – Regular exercise – Monitoring liver function with regular health check-ups |
| Associated Diseases | – Hepatitis B and C – Non-alcoholic fatty liver disease – Wilson’s disease – Hemochromatosis – Liver tumors |

Prof. Dr. Özgür KILIÇKESMEZ
Interventional Radiology / Interventional Neuroradiology
Prof. Dr. Kılıçkesmez holds the Turkish Radiology Competency Certificate, the Turkish Interventional Radiology Competency Certificate, Stroke Treatment Certification, and the European Board of Interventional Radiology (EBIR). In his academic career, he won the Siemens Radiology First Prize in 2008.
What Is Hepatomegaly?
Hepatomegaly refers to the condition where the liver grows beyond normal limits and can appear as a sign of many diseases. Various factors such as infections, tumors, exposure to toxins, and metabolic disorders often lead to liver enlargement. Derived from the Ancient Greek words “hepar” (liver) and “megas” (large), hepatomegaly has been an important subject of medical research. Changes in liver size offer clues about overall health, so hepatomegaly has long been carefully examined. Detecting this condition and determining the underlying cause is essential for effective treatment. Liver enlargement especially provides valuable information for understanding the diseases in which it develops.
What Are the Causes of Hepatomegaly?
Hepatomegaly can occur as a sign of various health problems. The main factors that can cause liver enlargement include:
Infectious causes:
- Viral hepatitis
- Parasitic infections
- Bacterial infections
Tumoral causes:
- Primary liver tumors
- Metastatic cancers
- Hematological cancers
Metabolic and storage diseases:
- Non-alcoholic fatty liver disease
- Hemochromatosis
- Wilson’s disease
- Glycogen storage diseases
- Amyloidosis
Vascular diseases:
- Heart failure
- Budd-Chiari syndrome
Inflammatory and autoimmune diseases:
- Primary sclerosing cholangitis
- Sarcoidosis
Toxic effects:
- Alcohol-related liver disease
- Drug-induced liver injury
Other causes:
- Polycystic liver disease
- Infiltrative diseases
Treatment for hepatomegaly is shaped according to the underlying cause. In the diagnostic process, physical examination, laboratory analyses, and imaging techniques are important for uncovering the cause of the enlargement. In some cases, a liver biopsy may be required. Treatment options include lifestyle changes, medication, and surgical intervention.
How Common Is Hepatomegaly?
Hepatomegaly is seen at different rates globally, depending on various diseases and lifestyle factors. Although it is difficult to determine the exact frequency of hepatomegaly worldwide, it is known to be common, especially in association with certain diseases and conditions.
Western countries:
- Alcoholic liver disease
- Non-alcoholic fatty liver disease (MASLD)
- Related to alcohol use, obesity, and diabetes
Asia:
- High rates of MASLD
- South Asia 33.8%, Southeast Asia 33.1%, East Asia 29.7%
Age and Gender Differences:
- Children: Increase in hepatomegaly due to MASLD
- Adults: Metabolic diseases, alcohol, and viral hepatitis
Associated diseases:
- Metabolic issues: MASLD, NASH
- Infections: Schistosomiasis
- Alcohol: Chronic consumption
The prevalence of hepatomegaly varies depending on age, gender, and regional factors. Especially in societies with increasing obesity, hepatomegaly due to MASLD is becoming more common, while in some developing regions, hepatomegaly due to infectious diseases is more frequently observed.
How Does Hepatomegaly Develop?
Hepatomegaly, or liver enlargement, occurs through different mechanisms, each affecting the specific function and structure of the liver. The main processes leading to liver enlargement are related to cellular proliferation, intra- and extracellular accumulation, vascular obstruction, inflammation, and invasive diseases.
Cellular invasion:
- Cancer types
- Infections
Intracellular accumulation:
- Glycogen storage diseases
- Fatty liver
- Iron overload
Expansion of extracellular matrix:
- Chronic liver diseases
- Cirrhosis
Vascular obstruction and increased pressure:
- Right heart failure
- Budd-Chiari syndrome
Inflammatory processes:
- Acute hepatitis
- Chronic hepatitis
Invasive diseases:
- Amyloidosis
- Sarcoidosis
Each of these processes that cause hepatomegaly leads to significant changes in the structure and function of the liver, resulting in organ enlargement.
What Are the Symptoms of Hepatomegaly?
Hepatomegaly presents with symptoms that arise when the liver exceeds its normal size. These symptoms may vary depending on the severity of the disease and the underlying cause. Symptoms include:
- Feeling of fullness and pressure in the abdominal area
- Yellowing of the skin and eyes
- Fatigue and low energy
- Nausea and loss of appetite
- Unintentional weight loss
- Itching (pruritus)
- Swelling and edema in the body
- Easy bruising and bleeding
- Mental confusion and disorientation
- Dark-colored urine and pale stools
Liver enlargement especially causes a feeling of fullness in the upper right abdomen, leading to discomfort. Yellowing of the skin is related to problems in the liver’s ability to process bilirubin, which becomes noticeable in advanced stages. Decreased protein synthesis by the liver can cause fluid accumulation and edema, particularly in the legs. Insufficient production of clotting factors leads to easy bruising and bleeding. A decrease in the liver’s ability to clear toxins can result in mental confusion, affecting daily decision-making.
How Is Hepatomegaly Diagnosed?
The diagnosis of hepatomegaly requires a detailed medical evaluation. First, the patient’s history is carefully reviewed; information such as alcohol use, regular medications, exposure to toxic substances, and family history of liver disease is collected. This step is important for determining possible risk factors. During physical examination, the liver is evaluated by palpation, and it is checked whether the liver extends below the right costal margin.
Among imaging methods, abdominal ultrasonography is the first preferred quick and non-invasive method to determine liver enlargement. Ultrasonography can show both the size of the liver and changes in its tissue. In more complex cases, advanced techniques such as computed tomography (CT) and magnetic resonance imaging (MRI) are used. These methods allow a detailed examination of the sectional structure of the liver and help assess possible masses.
In addition to clinical evaluation, laboratory tests provide valuable information in diagnosing hepatomegaly. Liver function tests give information about the functioning of the liver. Parameters such as serum aminotransferases (AST, ALT), alkaline phosphatase, and bilirubin levels are evaluated. Serological tests for viral hepatitis and autoimmune diseases may also be performed. A complete blood count (CBC) is used to investigate findings such as anemia, leukopenia, or thrombocytopenia.
A liver biopsy may be performed if necessary in diagnosis. Biopsy involves taking a tissue sample from the liver for microscopic examination, especially when a definitive diagnosis cannot be made with other methods. Additional techniques such as ERCP and MRCP may be used to assess the condition of the bile ducts. Doppler ultrasonography checks hepatic blood flow and detects vascular abnormalities.
How Is Hepatomegaly Treated?
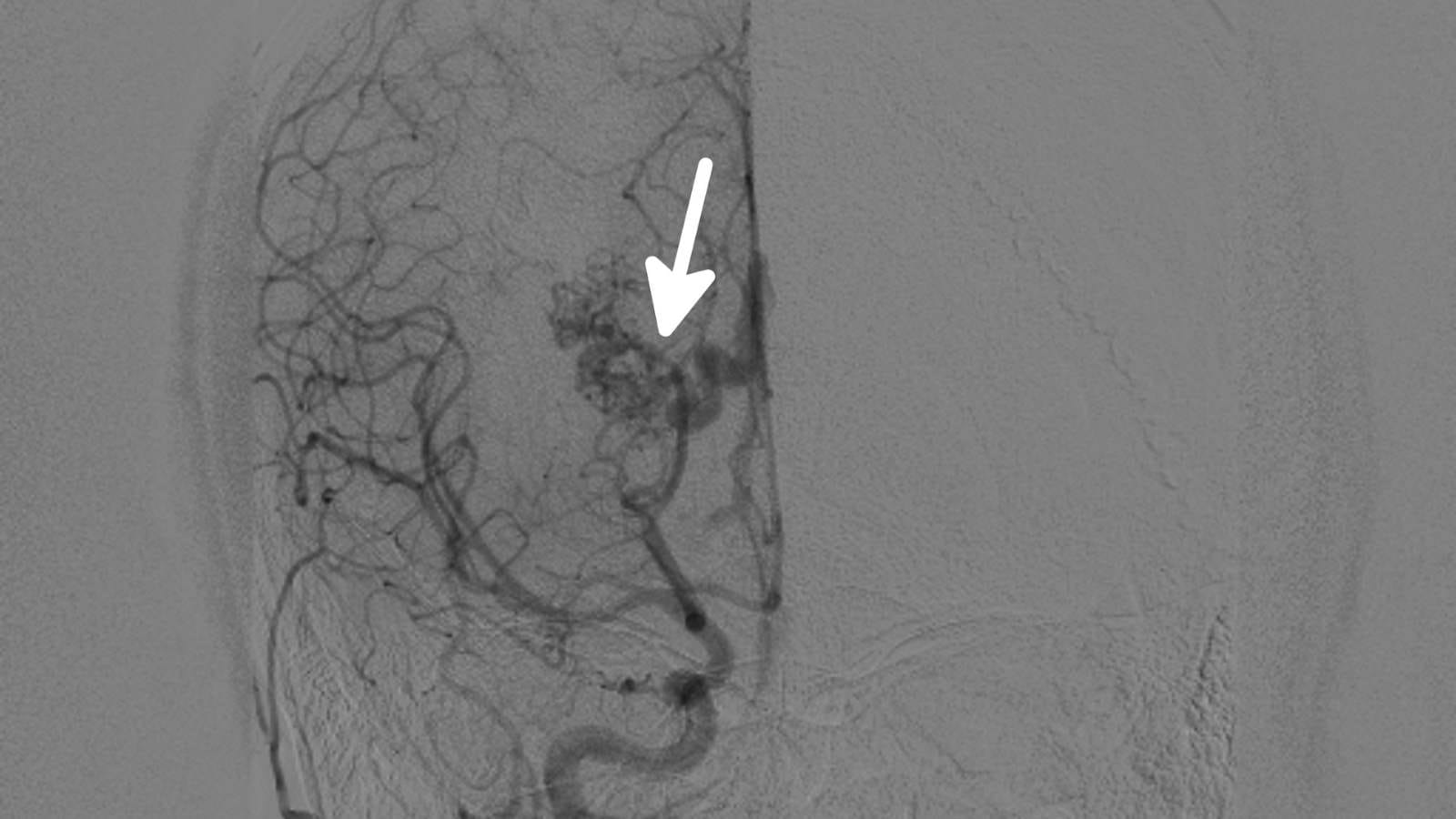
Interventional radiology techniques play an important role in the treatment of hepatomegaly depending on the underlying cause. These methods are generally non-invasive or minimally invasive procedures, performed to relieve symptoms caused by liver enlargement and support organ function. The main interventional radiology methods used in treatment include:
- TIPS procedure
- IVC stenting
- Portal Vein Embolization (PVE)
- Transarterial Embolization (TAE)
- Transarterial Chemoembolization (TACE)
- Percutaneous ablation techniques (RFA, MWA)
These treatments are carefully selected according to the patient’s condition and performed by a multidisciplinary team. Especially in specific conditions such as liver cirrhosis, polycystic liver disease, or giant liver tumors, these interventional methods stand out among treatment options.
What Are the Complications of Hepatomegaly?
Hepatomegaly is a condition that develops in association with various diseases, and if not treated in time, can lead to serious complications. Liver enlargement can cause functional disorders of the organ, affecting many systems in the body. Main complications that may arise from hepatomegaly include:
- Liver failure
- Bleeding tendency
- Increased risk of infection
- Development of cirrhosis
- Portal hypertension
- Hepatic coma
- Ascites (abdominal fluid accumulation)
- Varices
Liver failure is a serious complication that may be seen in the advanced stages of hepatomegaly. In this condition, the liver cannot adequately clear toxins from the body, causing dysfunction in other organs. The tendency to bleed increases because of insufficient production of clotting factors, leading to serious bleeding even with minor injuries.
Portal hypertension occurs when blood flow through the liver is blocked and can cause the development of varices. Esophageal varices in particular can increase the risk of bleeding and be life-threatening. Ascites is manifested as fluid accumulation in the abdominal cavity, causing severe discomfort.
Another important complication of hepatomegaly is hepatic coma, which results from severe loss of liver function and leads to accumulation of toxic substances in the brain, causing loss of consciousness. Early identification of the factors causing hepatomegaly and the implementation of appropriate treatment plans are vital to prevent such complications.
When Can Hepatomegaly Be Treated?
The treatment of hepatomegaly is generally planned according to the underlying cause and the patient’s general condition. During this planning, it is considered whether the mass causes symptoms, poses a risk of complications such as bleeding or infection, or has malignant transformation potential. If hepatomegaly causes serious symptoms and risks, surgical or interventional treatment methods are considered.
Situations requiring treatment include:
- Symptomatic lesions
- Masses with risk of bleeding
- Kasabach-Merritt syndrome
- Rapidly growing masses
- Lesions with potential for malignant transformation
- Lesions causing biliary obstruction
- Cases not responding to conservative treatment
In such cases, not only the size of the mass but also its impact on quality of life is considered. For example, large hemangiomas and rapidly growing adenomas may require intervention due to severe pain, pressure, and liver function impairment. Minimally invasive interventions such as transarterial embolization (TAE) and radiofrequency ablation (RFA) stand out among treatment options.
Interventional procedures minimize the surgical risks for the patient while effectively preventing complications and alleviating symptoms. For each case, multidisciplinary evaluation and monitoring during the treatment process are important to determine the most appropriate treatment method.
When Is Hepatomegaly Treatment Not Possible?
In some cases, hepatomegaly treatment cannot be performed due to the risks it may pose to the patient. Especially interventional treatments such as liver biopsy, transarterial chemoembolization (TACE), and portal vein embolization (PVE) are not preferred under certain health conditions. The patient’s current disease state, bleeding tendency, and other organ functions may limit treatment options. It is not performed in the following situations:
- Coagulation disorders
- Presence of ascites
- Possibility of movement during the procedure
- Extrahepatic bile duct obstruction
- Advanced liver failure
- Portal vein thrombosis
- Renal failure
- Severe cardiopulmonary disease
- Portal hypertension
- Total lobar portal vein obstruction
- Extrahepatic metastatic disease
- Insufficient liver volume
- Severe comorbid conditions (e.g., sepsis)
With these contraindications in mind, each patient is evaluated individually. In this way, both risks are minimized during treatment and the success of interventional treatment methods is increased.
What Is the Recovery Process of Hepatomegaly?
The recovery process after interventional procedures for hepatomegaly varies depending on the chosen treatment method and the patient’s general health. During recovery, pain management, monitoring of side effects, and control of possible complications are important.
Main points to consider during recovery:
- Pain and fever after transarterial embolization
- Mild bleeding risk after percutaneous ablation
- Possibility of hepatic encephalopathy after TIPS
- Early mobilization and nutrition with ERAS protocols
- Pain management with thoracic epidural analgesia
- Liver support with MARS system if needed
With ERAS protocols, rapid progress can be achieved in the recovery process of patients treated for hepatomegaly. These protocols help reduce pain and prevent complications after surgery. Pain management techniques used after surgery increase patient comfort and speed up the healing process. If liver function support is needed, systems such as MARS can be used to make the recovery process safer.
How Can Hepatomegaly Be Prevented?
A healthy lifestyle and preventive measures play a major role in preventing hepatomegaly (liver enlargement). Certain lifestyle changes and habits can be effective in preventing this condition. Prevention methods include:
- Reducing alcohol consumption
- Regular exercise
- Maintaining an ideal weight
- Adopting a balanced and nutritious diet
- Getting hepatitis A and B vaccines
- Avoiding unnecessary medications
- Limiting exposure to environmental toxins
- Keeping underlying diseases under control
These measures not only reduce the risk of hepatomegaly but also ensure that the liver works healthily and efficiently. The liver’s functions in filtering toxins and storing energy are vital for overall body health. Therefore, taking preventive steps for liver health not only lowers the risk of hepatomegaly but also supports the overall functioning of the body.
Frequently Asked Questions
What diseases can hepatomegaly indicate?
Hepatomegaly (enlarged liver) can be a sign of liver diseases such as hepatitis, cirrhosis, fatty liver disease, and liver cancer; infections such as mononucleosis, malaria, and schistosomiasis; genetic disorders such as hemochromatosis and Wilson’s disease; heart and vascular problems such as congestive heart failure and Budd-Chiari syndrome; and cancers such as leukemia and lymphoma. In Western countries, non-alcoholic steatohepatitis (NASH) due to obesity and type II diabetes is a common cause. Schistosomiasis, which affects more than 200 million people worldwide, is one of the most common causes of liver enlargement globally.
How is liver enlargement diagnosed?
Hepatomegaly, or liver enlargement, is diagnosed with physical examination, imaging methods, and laboratory tests. In physical examination, doctors assess liver size by palpation and percussion, and note any tenderness or irregularities. Imaging methods such as ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) provide detailed information on the liver’s size and structure. For example, in a study of 2,080 people, a liver size exceeding 16 cm along the midclavicular line was found in 12% of participants. Laboratory tests such as liver function tests can detect underlying conditions by measuring enzyme levels, such as viral hepatitis. In some cases, a liver biopsy may be performed to help identify liver diseases.
What are the most common causes of hepatomegaly?
The most common causes of hepatomegaly (liver enlargement) are non-alcoholic fatty liver disease (NAFLD), which occurs in about 25% of the world’s population, and alcoholic liver disease, which accounts for about 50% of liver diseases in Western countries. Viral hepatitis, especially hepatitis B and C, causes more than 1 million deaths worldwide each year. About 15% of people with congestive heart failure develop liver enlargement. Among metabolic disorders, hemochromatosis (1 in 200 people) and Wilson’s disease (1 in 30,000) are rarer causes. Infectious diseases such as schistosomiasis affect more than 200 million people worldwide and often cause hepatomegaly. In addition, liver malignancies such as metastatic cancer and primary liver cancer are important causes; liver cancer is the fourth most common cause of cancer-related deaths worldwide.
What treatment methods are applied for liver enlargement?
Treatment for hepatomegaly (liver enlargement) depends on the underlying cause. For example, for non-alcoholic fatty liver disease, weight loss, dietary changes, and increased physical activity are recommended. In alcoholic liver disease, complete cessation of alcohol use is vital. Drugs may be prescribed for conditions such as hepatitis, and factors such as diabetes and high cholesterol may need to be controlled. Regular blood tests and imaging studies are needed to assess liver function and monitor disease progression. In advanced cases such as severe cirrhosis, liver transplantation may be considered. The treatment plan should always be discussed with a healthcare professional.
What nutritional recommendations should be followed to prevent hepatomegaly?
To prevent hepatomegaly, a balanced diet including plenty of fruits, vegetables, whole grains, and lean proteins should be preferred, while saturated fats, trans fats, and refined sugars should be avoided. Fiber-rich legumes and whole grains support digestion and help reduce liver fat. Excessive alcohol consumption should be avoided, as this can lead to liver enlargement. Regular physical activity, combined with a healthy diet, also helps protect liver health. For personalized recommendations, consulting a healthcare provider is advised.

Girişimsel Radyoloji ve Nöroradyoloji Uzmanı Prof. Dr. Özgür Kılıçkesmez, 1997 yılında Cerrahpaşa Tıp Fakültesi’nden mezun oldu. Uzmanlık eğitimini İstanbul Eğitim ve Araştırma Hastanesi’nde tamamladı. Londra’da girişimsel radyoloji ve onkoloji alanında eğitim aldı. İstanbul Çam ve Sakura Şehir Hastanesi’nde girişimsel radyoloji bölümünü kurdu ve 2020 yılında profesör oldu. Çok sayıda uluslararası ödül ve sertifikaya sahip olan Kılıçkesmez’in 150’den fazla bilimsel yayını bulunmakta ve 1500’den fazla atıf almıştır. Halen Medicana Ataköy Hastanesi’nde görev yapmaktadır.







Vaka Örnekleri