Anaplastic thyroid cancer is a rare but highly aggressive malignancy of the thyroid gland. It progresses rapidly, often presenting with a large neck mass, difficulty breathing, and swallowing problems, requiring urgent medical intervention.
Unlike other thyroid cancers, anaplastic carcinoma has a poor prognosis due to its fast spread and resistance to standard treatments. Surgery is rarely curative, and most patients require combined therapy for disease control.
Treatment often involves radiation and chemotherapy to slow tumor progression. Newer targeted therapies and immunotherapy approaches are being studied, offering potential for improved survival in selected patients.
Early diagnosis and multidisciplinary care are critical. Rapid referral to specialized cancer centers maximizes treatment options and provides the best chance of symptom relief and extended survival.
| Disease Name | Anaplastic Thyroid Cancer (ATC) |
| Definition | The rarest and most aggressive form of thyroid cancer; tends to grow and spread rapidly and is often diagnosed at an advanced age. |
| Symptoms | Rapidly growing neck mass, difficulty swallowing and breathing, hoarseness, neck pain, cough, and symptoms such as paralysis of the vocal cords. |
| Causes | Transformation of other types of thyroid cancer, advanced age, exposure to radiation; however, the exact causes are not fully known. |
| Risk Factors | Advanced age, female gender, history of long-term goiter, long-standing nodules in the thyroid, history of radiation exposure. |
| Diagnostic Methods | Physical examination, thyroid ultrasound, fine-needle aspiration biopsy, CT and MRI imaging, PET scan (to assess spread), serum T3, T4, TSH levels. |
| Treatment Methods | Surgical intervention (often limited), radiotherapy and chemotherapy, targeted therapy; palliative treatments are also used to manage pain and symptoms. |
| Prognosis | Very poor; the disease is usually diagnosed at an advanced stage and progresses rapidly despite treatment. Survival time is generally short. |
| Follow-up and Monitoring | Intensive care support, supportive treatments to relieve symptoms; in case of tumor spread, follow-up with advanced imaging methods. |
| Complications | Can quickly metastasize to lungs, bones, and other organs; airway obstruction, difficulty swallowing, severe functional disorders. |
| Prevention Methods | There is no specific prevention method; however, regular check-ups for those with a history of goiter or thyroid nodules and early screening in high-risk groups are important. |
| Response to Treatment | Generally resistant to treatment; despite multiple treatment options, it is difficult to control and palliative approaches focused on symptom management are prioritized. |
Prof. Dr. Özgür KILIÇKESMEZ Prof. Dr. Kılıçkesmez holds the Turkish Radiology Competency Certificate, the Turkish Interventional Radiology Competency Certificate, Stroke Treatment Certification, and the European Board of Interventional Radiology (EBIR). In his academic career, he won the Siemens Radiology First Prize in 2008.
Interventional Radiology / Interventional Neuroradiology
What Is Anaplastic Thyroid Cancer?
Anaplastic thyroid cancer is a rare and extremely aggressive type among thyroid cancers. Although it accounts for less than 2% of thyroid cancer cases, it progresses rapidly and leads to poor outcomes. It usually presents as a hard and fixed mass in the neck, which can cause difficulty swallowing and breathing. The most notable feature of the disease is the rapid growth of tumors, invasion of surrounding tissues, and tendency to metastasize to distant organs. Therefore, at the time of diagnosis, life expectancy for patients with anaplastic thyroid cancer is generally limited.
What Are the Causes of Anaplastic Thyroid Cancer?
The causes of anaplastic thyroid cancer can be explained by a complex interaction of both genetic and environmental factors. One of the most important genetic factors in the development of this cancer is mutations in the TP53 gene. TP53 regulates the cell cycle and controls apoptosis. These mutations contribute to uncontrolled cell growth. In addition, mutations in the BRAF gene, especially the BRAF V600E mutation, affect cell proliferation and accelerate tumor growth.
The genomic structure of anaplastic thyroid cancer is also characterized by copy number variations. Copy number changes include large chromosomal alterations that disrupt the genetic balance of cells. In this context, amplification of certain chromosomal regions is frequently observed in cancer cells. Especially the 5p and 20q chromosomal regions contain critical genes that regulate the cell cycle and apoptosis.
- Chromosome 5p: Contains genes related to cell cycle progression such as SKP2 and E2F1.
- Chromosome 20q: Includes genes such as BCL2L1 that affect apoptosis and the PI3K-Akt signaling pathway.
Environmental and clinical factors also play an important role in the development of this disease. Individuals who have previously had papillary or follicular thyroid cancer and those exposed to radiation have an increased risk of progressing to anaplastic thyroid cancer. Advanced age is another significant risk factor for this type of cancer. It is more common in individuals aged 65 and older.
The combination of these genetic and environmental factors results in the fatal nature of anaplastic thyroid cancer.
*We recommend filling out all fields so we can respond in the best possible way.
How Common Is Anaplastic Thyroid Cancer?
Anaplastic thyroid cancer (ATC) is extremely rare but is one of the most fatal forms of thyroid cancer. Globally, about 1 to 2 cases of ATC are reported per million people each year. This cancer type accounts for only 1-2% of all thyroid cancer cases. However, the aggressive nature of ATC and its resistance to current treatments make it a disproportionate cause of thyroid cancer deaths. ATC, which is more common in older adults, is typically diagnosed in individuals between the ages of 65 and 70.
Demographically, ATC shows a more balanced gender distribution compared to other types of thyroid cancer. Although the incidence in women is slightly higher, rates are similar in both men and women.
- Global incidence: Approximately 1 to 2 cases per million people annually
- Gender distribution: Slightly more common in women
- Age distribution: Average diagnosis age is between 65-70 years
Geographically, iodine deficiency regions have been observed to have higher rates of thyroid cancer. In regions with limited access to healthcare, delayed diagnosis and inadequate treatment may also increase the incidence of ATC. A significant portion of ATC cases develop from pre-existing papillary or follicular thyroid cancers. Therefore, individuals previously diagnosed with differentiated thyroid cancer are at higher risk of developing ATC.
What Is the Formation Process of Anaplastic Thyroid Cancer?
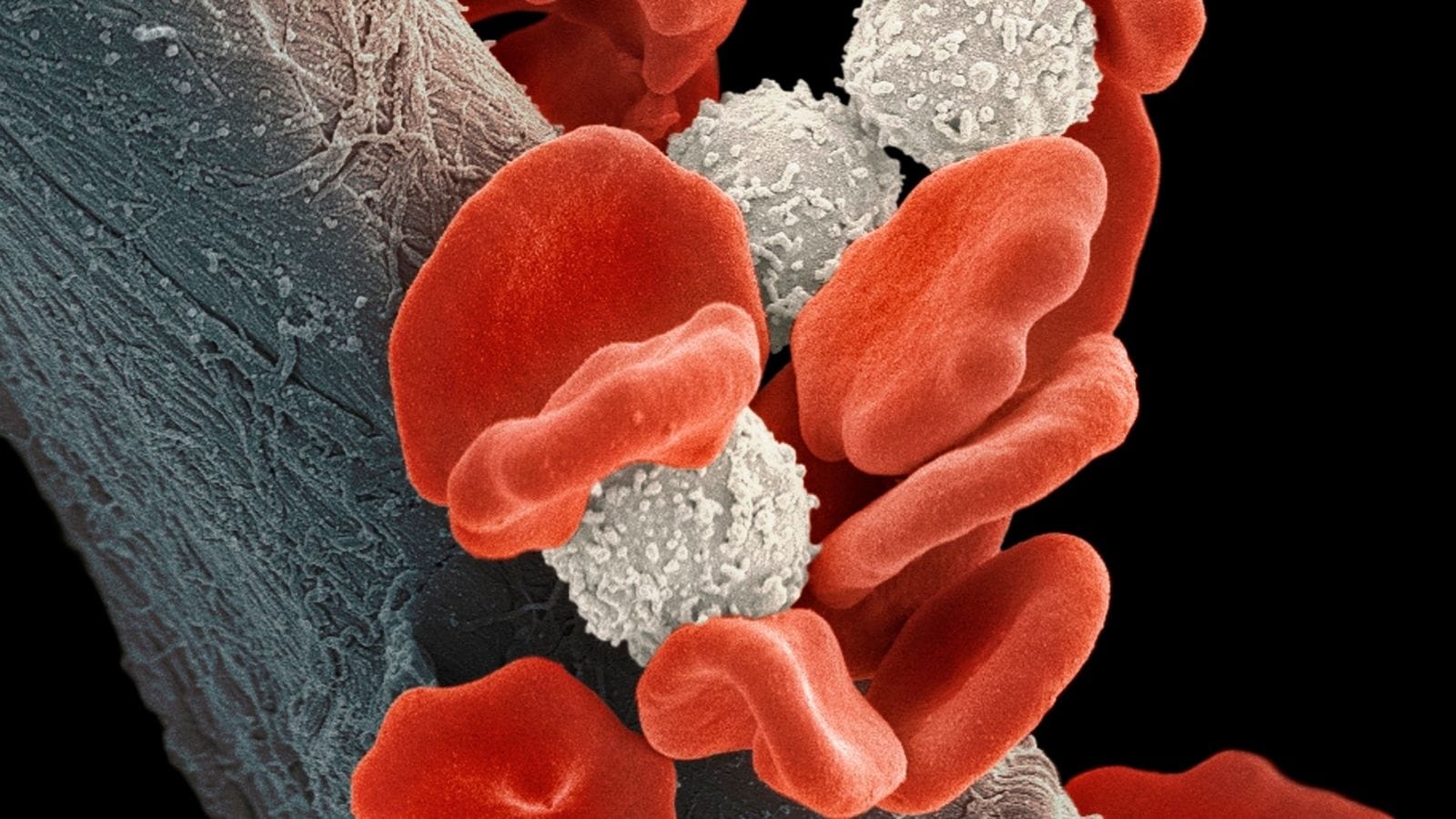
Anaplastic thyroid cancer develops as a result of a multi-step process characterized by genetic mutations and loss of cellular differentiation. It generally arises from differentiated thyroid cancers such as papillary or follicular thyroid carcinomas through a process of dedifferentiation. This process is accelerated by the accumulation of genetic and epigenetic changes that cause thyroid cells to lose their normal function.
Certain genetic mutations, in particular, increase the aggressive biological behavior of ATC. These include:
- TP53 mutation: This tumor suppressor gene mutation leads to uncontrolled cell growth.
- BRAFV600E mutation: Occurs in proto-oncogenes, especially in the BRAF gene, and accelerates tumor formation.
- CDKN2A mutation: Changes in these genes that regulate the cell cycle facilitate the proliferation of cancer cells.
- PIK3CA mutation: Activates the PI3K/AKT pathway and supports the survival of cancer cells.
In addition to these genetic changes, copy number variations on chromosomes 5p and 20q and chromosomal instability increase the invasive capacity of the tumor. Due to the dysregulated tumor microenvironment in ATC, overactivation of signaling pathways such as MAPK and JAK/STAT further increases its aggressiveness. In addition, long non-coding RNAs such as LINC00312 and H19 affect the proliferation and metastasis of cancer cells.
What Are the Symptoms of Anaplastic Thyroid Cancer?
Anaplastic thyroid cancer is known as a rare and highly aggressive type of thyroid cancer. Symptoms usually appear rapidly and the progression of the disease is also very fast. Most patients begin to experience severe symptoms within a few weeks, and these symptoms intensify in parallel with the rate of disease spread. The most common symptoms of this cancer type include:
- Neck mass or swelling: A rapidly growing, externally visible mass in the neck is a primary symptom.
- Difficulty swallowing (dysphagia): As the tumor is located near the esophagus, its growth may cause swallowing difficulties.
- Shortness of breath (dyspnea): The tumor can press against the trachea, causing difficulty breathing and wheezing.
- Hoarseness or voice changes: The cancer may damage the nerves affecting the vocal cords, causing hoarseness or voice changes.
- Neck pain: The expansion of the tumor may cause pain in the neck region.
- Cough or bloody cough: Persistent cough or, rarely, bloody coughing may occur.
- Fatigue and weakness: As the disease progresses, general fatigue and weight loss may develop.
- Lymph node enlargement: Enlargement of lymph nodes in the neck is a common finding.
- Obstructive symptoms: Compression of the trachea or esophagus can increase breathing and swallowing difficulties.
How Is Anaplastic Thyroid Cancer Diagnosed?
The diagnosis of anaplastic thyroid cancer is made by combining various clinical imaging and histopathological methods. The disease usually presents as a rapidly growing neck mass, often accompanied by symptoms such as dysphagia, hoarseness, or difficulty breathing. Most patients are diagnosed at advanced stages due to the aggressive nature of the cancer, which often results in local invasion and distant metastases.
Imaging techniques play a significant role in assessing the extent and size of the tumor. Commonly used imaging methods include:
- CT scans: Help assess the size of the tumor and its spread to adjacent tissues.
- MRI: Provides more detailed examination of soft tissue involvement.
- FDG-PET scans: Detects the spread of metastatic disease to distant organs such as lungs and bones.
Definitive diagnosis is made by histopathological analysis of a sample taken by fine-needle aspiration biopsy. This analysis confirms the presence of poorly differentiated malignant cells characteristic of ATC. Histopathological features include marked pleomorphism and necrosis.
Additionally, molecular and genetic tests are becoming increasingly important in the diagnosis of ATC. Genetic analyses identifying mutations such as TP53, BRAF, and RAS both confirm the diagnosis and guide the treatment process.
How Is Anaplastic Thyroid Cancer Treated?
Although various methods are used in the treatment of anaplastic thyroid cancer (ATC), the results are generally limited. Treatment is mostly palliative and aims to control the disease and improve the patient’s quality of life. Interventional radiology, targeted therapies, and immunotherapies are among the treatment options used for this type of cancer.
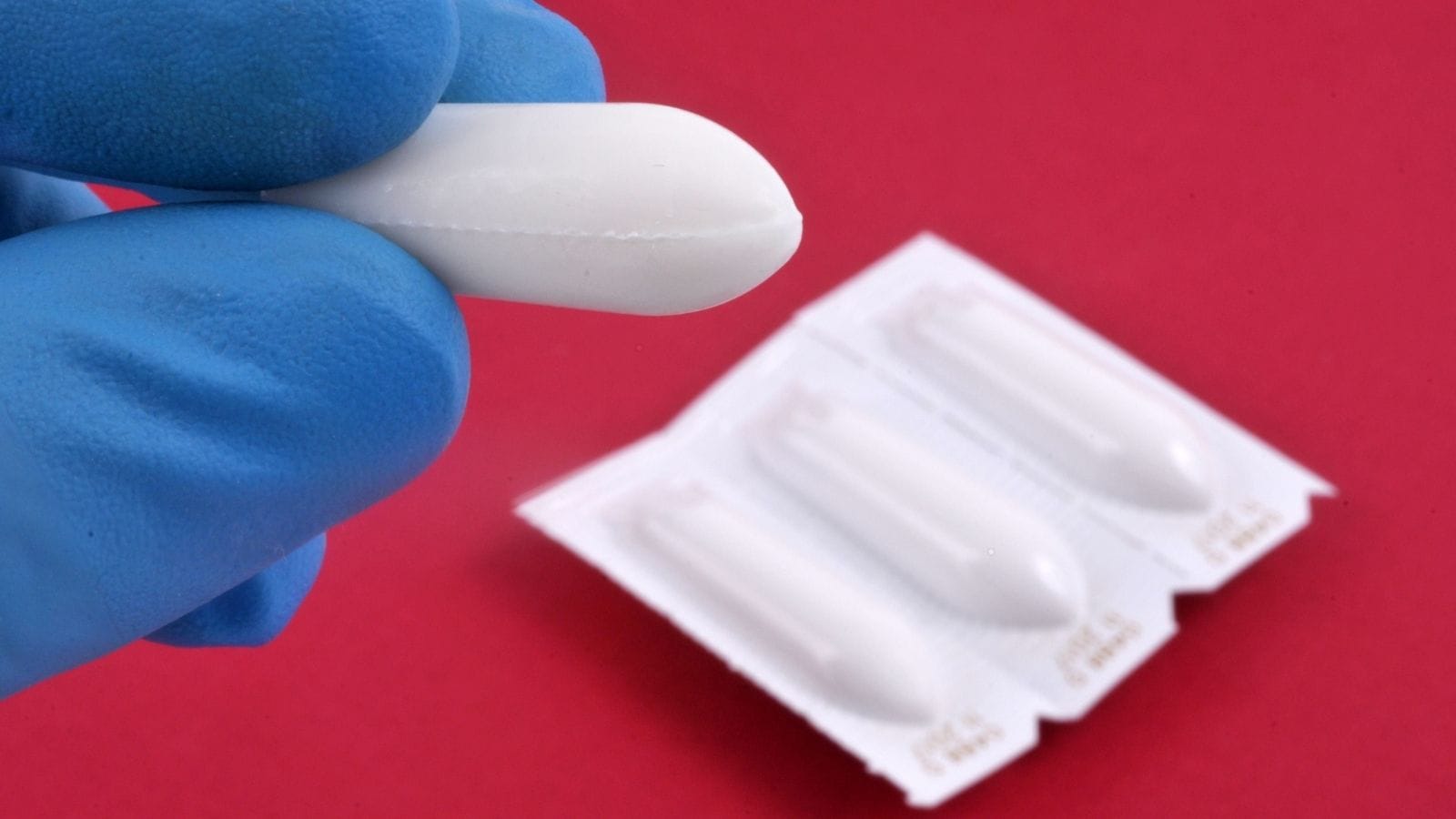
Interventional radiology plays an important role, especially in patients who are not candidates for surgery. This method tries to control tumor growth and alleviate symptoms. Techniques such as radiofrequency ablation (RFA) and percutaneous ethanol injection (PEI) are used for this purpose.
- Radiofrequency ablation (RFA): Uses thermal energy to destroy tumor cells.
- Percutaneous ethanol injection (PEI): Ethanol is injected into the tumor to induce tumor necrosis.
- Thermal ablation: Methods such as microwave ablation or cryoablation are used to target metastases.
Targeted therapies attempt to block specific cellular processes such as the MAPK and PI3K pathways. Although these therapies aim to halt tumor growth, their effects remain limited.
Finally, immunotherapies activate the immune system against cancer. However, due to the rapid progression of ATC, the effects of these therapies are usually limited.
A multidisciplinary approach is essential in ATC treatment. Interventional radiology, targeted therapies, and immunotherapies are often combined to achieve better results.
What Are the Risk Factors for Anaplastic Thyroid Cancer?
Various risk factors for anaplastic thyroid cancer include genetic, environmental, and lifestyle elements. This type of cancer is more common in older individuals, especially those over the age of 60. Although it is more frequent in men, the disease course is generally more severe in this gender.
Pre-existing thyroid diseases also increase the risk of developing ATC. Multinodular goiter or a history of long-term thyroid disorders places individuals at greater risk. In addition, differentiated thyroid cancers can transform into anaplastic thyroid cancer over time through genetic mutations.
Genetic mutations also play an important role in the development of this cancer. Especially mutations in genes such as BRAF, TP53, and RAS contribute to the aggressive nature of the disease and its resistance to treatment.
- Age and gender: Usually seen in individuals over 60 and more frequent in men.
- Pre-existing thyroid diseases: Those with multinodular goiter or a history of differentiated thyroid cancer are at risk.
- Genetic mutations: Mutations in genes such as BRAF, TP53, and RAS are involved in disease development.
- Radiation exposure: Previous radiation therapy to the head and neck increases risk.
- Environmental factors: Living in iodine-deficient areas may pose a risk.
- Lifestyle: Factors such as smoking and obesity also increase the risk.
When Can Anaplastic Thyroid Cancer Treatment Be Performed?
Anaplastic thyroid cancer treatment is usually applied in cases where surgical options are limited or the tumor cannot be resected. Interventional radiology (IR) plays an important role in the management of this disease and offers different treatment approaches. These approaches are evaluated according to the level of disease progression and the patient’s symptoms.
In particular, IR techniques come into play in the following situations:
- Palliative management of symptoms: Interventional radiology is used to relieve symptoms such as shortness of breath, difficulty swallowing, and pain caused by rapidly growing tumors. Placement of a tracheal or esophageal stent can reduce compression effects.
- Ablative therapies: In localized tumors where surgery is not possible, thermal techniques such as radiofrequency ablation, cryoablation, or microwave ablation may be preferred. These methods can provide local control of the disease.
- Embolization: In inoperable or non-radiotherapy candidates, transarterial embolization can be used to cut off the blood supply to the tumor. It can also be used preoperatively to reduce bleeding risk.
- Image-guided biopsy: In cases where the tumor is deeply located, ultrasound or CT-guided needle biopsy can be performed to obtain a diagnostic sample. This method is necessary for an accurate diagnosis.
- Management of vascular involvement: In cases where the tumor spreads to major vessels, stenting or embolization can be performed to prevent vascular obstruction or rupture.
When Is Anaplastic Thyroid Cancer Treatment Not Possible?
Anaplastic thyroid cancer treatment may not always be feasible. Interventional radiology treatments are generally palliative approaches aimed at alleviating symptoms, but there are cases where they cannot be applied. The main barrier is extensive disease involvement. If the tumor invades the trachea, esophagus, or major blood vessels, interventional procedures carry the risk of bleeding or organ damage. Therefore, treatment may not be possible in such cases. Additionally, the patient’s poor performance status is an important factor. Patients with an ECOG score of 3 or higher may not tolerate the anesthesia required for procedures. For this reason, interventional radiology is not preferred in these patients.
In addition, patients with coagulation disorders may not be suitable for interventional radiology treatments. The risk of complications is high in patients on anticoagulant therapy or those with a tendency to bleed. ATC patients are likely to experience coagulation problems due to causes such as liver metastases. Furthermore, conditions such as infection or sepsis are serious contraindications for interventional treatments.
Finally, lack of tumor controllability is also an important factor. In rapidly growing and spreading ATC, it may be difficult to localize the tumor. This makes the application of methods such as radiofrequency ablation or cryoablation challenging. In addition, patients who have previously received extensive radiation or become radiation-sensitive may not benefit from these treatment methods.
What Is the Recovery Process After Anaplastic Thyroid Cancer Treatment?
The recovery process after interventional radiology in the treatment of anaplastic thyroid cancer requires considerable attention. Nevertheless, it aims to improve patients’ quality of life and extend survival time. The recovery process varies from patient to patient and depends on the following factors:
- Tumor location and size
- How successful symptom control is
- The patient’s general health status and age
The post-treatment monitoring process is generally important. However, complications may occur. These complications include the risk of fistula formation, infection, or damage to surrounding tissues. Therefore, patients’ conditions should be carefully monitored and necessary precautions should be taken. In conclusion, the recovery process after interventional radiology is a complex process that requires a multidisciplinary approach. The effectiveness of the treatment process may vary depending on the patient’s individual characteristics.
How Can Anaplastic Thyroid Cancer Be Prevented?
Prevention of anaplastic thyroid cancer generally involves preventive measures related to differentiated thyroid cancers (DTC). Therefore, early diagnosis and treatment of these cancer types is of great importance. This helps prevent the development of cases that could potentially become anaplastic. Here are the strategies to follow in this process:
- Treatment of Differentiated Thyroid Cancer: Effective treatment of DTC plays a critical role in reducing the risk of ATC. This requires regular monitoring and early intervention.
- Screening and Genetic Testing: Genetic screening to identify potentially risky mutations helps direct patients to more aggressive treatment.
- Close Monitoring of High-Risk Patients: Regular monitoring of patients with genetic mutations or a history of thyroid cancer is important. This allows for early detection of any aggressive behavior.
- Targeted Therapy in Pre-cancerous Conditions: New generation targeted therapies can prevent the transformation of cancer into the anaplastic form. Early use of these therapies in high-risk patients is beneficial.
Frequently Asked Questions
How is anaplastic thyroid cancer different from other thyroid cancers?
Anaplastic thyroid cancer (ATC) is a rare and aggressive type of cancer, accounting for less than 2% of all thyroid cancer cases. Compared to the over 98% five-year survival rates for papillary and follicular thyroid cancers, the five-year survival rate for ATC is only 8%. It generally affects individuals over the age of 60 and is characterized by rapid growth and early metastasis, resulting in symptoms such as a rapidly growing neck mass, pain, and difficulty swallowing and breathing. Due to its aggressive nature, ATC is usually classified as stage IV at diagnosis, whereas other thyroid cancers are typically detected at earlier stages. Treatment options may include surgery, radiation, and chemotherapy, but prognosis is significantly worse compared to other thyroid cancers.
How quickly do symptoms develop in this cancer type?
Anaplastic thyroid cancer (ATC) progresses very rapidly, and symptoms usually develop within a few weeks. About 65% of patients experience symptoms in less than one month. The most common symptoms include a rapidly growing neck mass, pain, difficulty swallowing (dysphagia), difficulty breathing (dyspnea), hoarseness, and local invasion signs such as vocal cord paralysis. Due to its fast progression, ATC has usually metastasized at the time of diagnosis and any symptoms require immediate medical evaluation.
What treatment methods are used in anaplastic thyroid cancer?
Treatment of anaplastic thyroid cancer (ATC) includes combinations of surgery, radiotherapy, chemotherapy, targeted therapy, and immunotherapy. If the tumor can be completely removed, surgery is preferred. Radiotherapy, especially intensity-modulated radiotherapy, is often administered in combination with chemotherapy drugs such as doxorubicin or taxanes and platinum-based therapies. Molecular profiling has shown that the combination of dabrafenib and trametinib is effective in patients with the BRAF V600E mutation. Immunotherapies, especially in tumors with PD-L1 expression, are evaluated with drugs such as pembrolizumab and spartalizumab. Multimodal treatment approaches play a significant role in improving survival rates.
Why is the prognosis poor in this cancer type?
Anaplastic thyroid cancer (ATC) is an extremely aggressive disease with a median survival of about 4 months; the 6-month overall survival rate is 35%. Disease-specific mortality is 98-99%. Despite multiple treatment methods, the 1-year disease-specific survival rate is only around 20%. However, targeted therapies and immunotherapies in recent years have shown the potential to improve outcomes in some patients.
How effective are clinical trials in anaplastic thyroid cancer?
The effectiveness of clinical trials for anaplastic thyroid cancer (ATC) has increased in recent years with targeted therapies and multimodal approaches. Historically, the median overall survival for ATC was around 4 months, with a 6-month survival rate of 35% and disease-specific mortality rates between 98-99%. According to data from 2000-2019, 1-year survival rates increased from 35% to 59%, and 2-year survival rates from 18% to 42%. In particular, the combination of BRAF inhibitors (dabrafenib) and MEK inhibitors (trametinib) has shown significant efficacy in patients with BRAF V600E-mutant ATC. In addition, the inclusion of immunotherapies such as pembrolizumab is promising in increasing patient responses. However, ATC remains an extremely aggressive cancer type, and ongoing clinical research is focused on discovering new treatment combinations to further improve patient outcomes.

Girişimsel Radyoloji ve Nöroradyoloji Uzmanı Prof. Dr. Özgür Kılıçkesmez, 1997 yılında Cerrahpaşa Tıp Fakültesi’nden mezun oldu. Uzmanlık eğitimini İstanbul Eğitim ve Araştırma Hastanesi’nde tamamladı. Londra’da girişimsel radyoloji ve onkoloji alanında eğitim aldı. İstanbul Çam ve Sakura Şehir Hastanesi’nde girişimsel radyoloji bölümünü kurdu ve 2020 yılında profesör oldu. Çok sayıda uluslararası ödül ve sertifikaya sahip olan Kılıçkesmez’in 150’den fazla bilimsel yayını bulunmakta ve 1500’den fazla atıf almıştır. Halen Medicana Ataköy Hastanesi’nde görev yapmaktadır.







Vaka Örnekleri