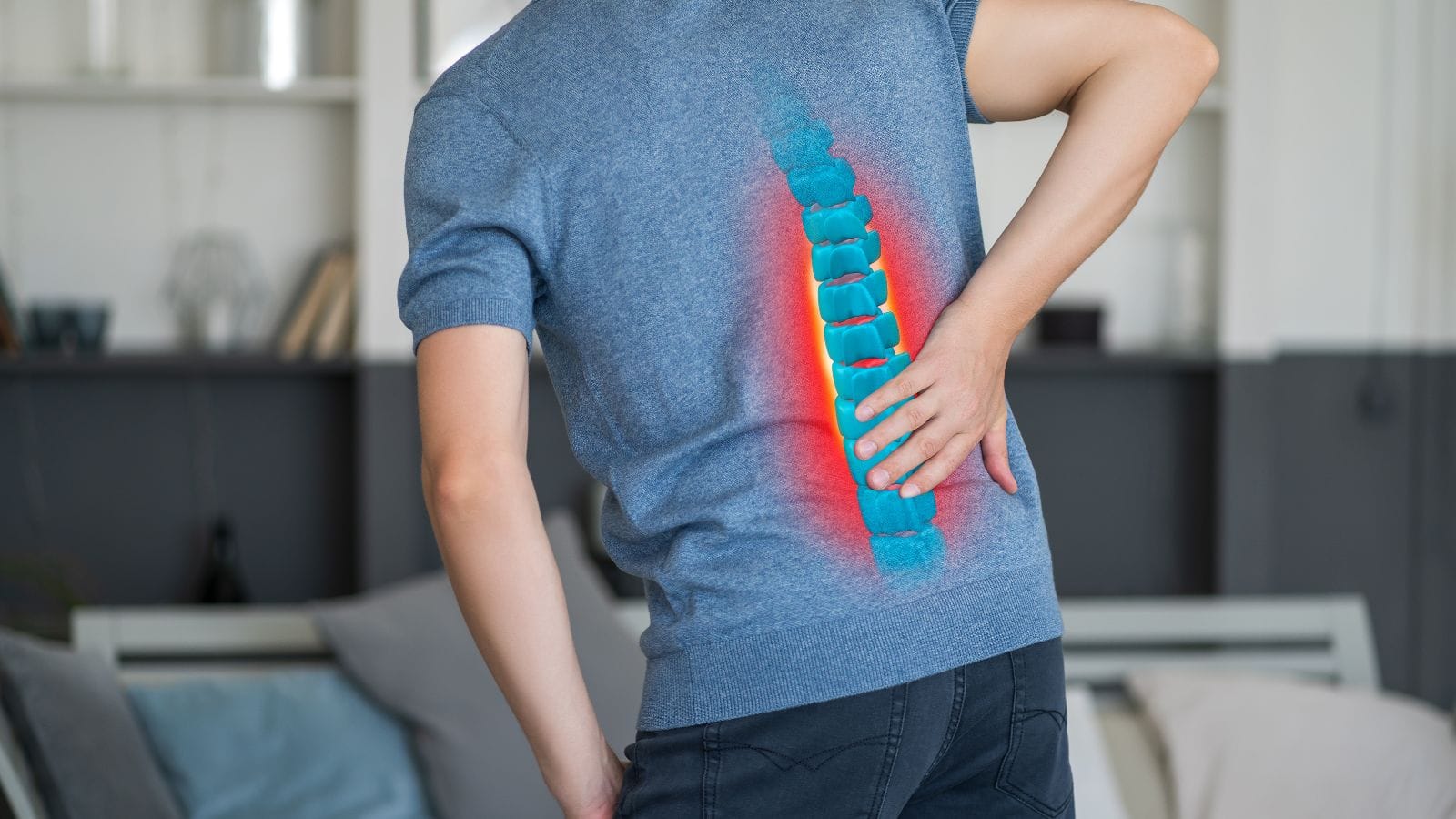
Lumbar hernia occurs when an intervertebral disc protrudes and compresses spinal nerves. This condition leads to symptoms such as low back pain, leg numbness, and sciatica.
Diagnosis involves clinical examination and imaging techniques like MRI, which reveal the extent of nerve compression and disc damage.
Conservative treatment includes rest, physical therapy, medication, and epidural injections. These methods help reduce inflammation and relieve nerve pressure.
Surgical or interventional options are considered for persistent or severe cases. Minimally invasive techniques such as microdiscectomy or radiofrequency therapy provide effective relief.
| Definition | – A herniated spinal disc is a condition where the jelly-like material inside a spinal disc pushes out through a tear, compressing nearby nerves. This pressure can cause pain, numbness, or muscle weakness along the affected nerve root. |
| Symptoms | – Low back and leg pain (sciatica) – Numbness or tingling in the leg – Muscle weakness (especially in the ankle or toes) – Pain worsening with movement – Loss of bladder or bowel control (emergency sign) |
| Causes | – Disc degeneration (age-related wear and tear) – Sudden strain or trauma – Heavy lifting – Poor posture or excessive load on the spine |
| Risk Factors | – Advanced age – Obesity – Heavy physical work or frequent lifting – Sedentary lifestyle – Family history of herniated discs |
| Diagnostic Methods | – Physical examination (nerve root tests, reflex evaluation) – Magnetic resonance imaging (MRI) – Computed tomography (CT) – Electromyography (EMG) (to assess nerve function) |
| Treatment Options | Conservative Treatment: – Painkillers and anti-inflammatory medications – Physical therapy – Epidural steroid injections – Rest (but avoid prolonged inactivity) – Nucleoplasty (regression therapy) Surgical Treatment: |
| Complications | – Permanent nerve damage – Chronic pain – Persistent muscle weakness – Loss of bladder or bowel control (cauda equina syndrome) |
| Prevention | – Regular exercise and strengthening back muscles – Maintaining a healthy weight – Practicing correct posture – Using proper lifting techniques (lifting with the knees) |
| Recovery Process | – Most cases improve within 4-6 weeks with conservative therapy. – Post-surgical recovery may take 4-12 weeks depending on the method used. |
| Emergency Signs | – Severe and persistent pain – Weakness in both legs – Loss of bladder or bowel control (requires urgent medical attention) |
What Is a Nerve-Compressing Lumbar Disc Herniation?
A nerve-compressing lumbar disc herniation occurs when the soft inner core of a disc pushes out through a tear in the tough outer layer, putting pressure on the nerves. This can lead to pain, numbness, or muscle weakness along the affected nerve’s path. It is most frequently seen in adults between the ages of 30 and 50 and may negatively impact quality of life as the herniation puts pressure on nerves.
What Causes Nerve-Compressing Disc Herniation?
Many factors contribute to herniated discs that compress nerves. Aging causes the disc to lose its strength and moisture, increasing the risk. Everyday traumas can also damage discs and compress nerves. Genetics may make some discs weaker than others. Additional contributing factors include:
- Repetitive movements
- Occupational strain
- Obesity
- Smoking
- Poor lifting techniques
- Physical inactivity
- Exposure to vibration
Jobs requiring prolonged sitting and inactivity can weaken the muscles that support the spine, further increasing the risk.
How Common Is Lumbar Disc Herniation?
This condition is common in people aged 30–59, and men are affected more often than women. Lifetime prevalence is about 10%, but symptomatic cases are limited to 5%. The most frequently affected spine levels are L4/L5 and L5/S1. Research indicates that herniated discs occur in 31.9% of those with back pain, and men are about twice as likely as women to develop it, especially in middle age.
How Does a Nerve-Compressing Herniated Disc Develop?
Disc herniation begins with gradual wear and loss of structure of the discs between the vertebrae. Discs are composed of a tough annulus fibrosus and a jelly-like nucleus pulposus. As we age, discs lose height and structural integrity, which leads to:
- Loss of disc moisture
- Reduced structural strength
- Weakening of the annulus fibrosus
- Formation of small tears
- Extrusion of the nucleus pulposus
The herniated disc may then press on nerve roots, triggering inflammation and pain—sometimes severe—down the back and legs. Inflammation chemicals, such as tumor necrosis factor-alpha, intensify the pain.
What Are the Symptoms?
Symptoms depend on the location and severity of nerve compression and may include:
Pain
- Sciatica-type pain radiating from the hip down the leg
- Sharp or persistent pain in the back or neck
Sensory Disorders
- Numbness in arms, legs, hands, or feet
- Tingling or pins-and-needles sensation
Muscle Weakness
- Difficulty lifting objects
- Weakness in fine motor skills
- Decreased reflexes
Autonomic Issues
- Bowel or bladder dysfunction
Movement and Coordination Problems
- Loss of balance
- Unsteady gait
- Muscle spasms in the back or neck
As the herniation progresses, symptoms may worsen, restricting daily activities. In severe cases, there is risk of falls, and bowel or bladder issues may require urgent care.
How Is It Diagnosed?
A comprehensive diagnosis includes:
- Medical history (onset and nature of pain, duration, and associated symptoms)
- Physical examination (testing muscle strength, sensory function, and reflexes)
- Observation (posture and gait)
- Palpation (checking for tenderness along the spine)
- Movement tests (to pinpoint pain sources)
- Provocative tests (such as straight leg raise)
- Imaging (MRI preferred, CT for bony details, myelography for complex cases)
- Electrodiagnostic tests (nerve conduction studies, EMG)
This multi-faceted approach is crucial for accurately identifying the herniated disc and planning the best treatment.
How Is It Treated?
Minimally invasive techniques are often used to reduce pressure on the nerve root when conservative treatment fails. These methods include:
- Epidural steroid injection
- Disc biacuplasty
- Percutaneous laser disc decompression (PLDD)
- Ozone therapy
- Endoscopic discectomy (surgery)
- Microscopic lumbar laminoplasty (surgery)
- Anterior cervical discectomy and fusion (ACDF) for cervical discs
The choice of treatment depends on overall health, the size of the herniation, and degree of nerve compression. A spine specialist will select the most appropriate method based on your unique needs.
Possible Complications
- Chronic pain
- Numbness in limbs
- Muscle weakness
- Loss of reflexes
- Movement restrictions
- Balance disorders
- Incontinence
- Bowel control loss
In advanced cases, cauda equina syndrome—a rare but serious condition—can develop, causing permanent loss of bowel and bladder control or even leg paralysis. Early intervention is key to avoiding complications.
When Is Treatment Necessary?
Interventional procedures are considered when conservative management fails or if there are severe neurological symptoms. Indications include persistent radiculopathy, neurological deficits, cauda equina syndrome, severe pain, recurrent herniation, or failed conservative therapy. Prompt treatment is vital to prevent permanent damage.
When Should Treatment Not Be Performed?
Certain situations may prevent interventional treatments:
Epidural steroid injections:
- Active infection
- Bleeding disorders
- Allergy to corticosteroids
- Poorly controlled diabetes
- Severe spinal deformities
- Pregnancy
Spinal cord stimulation:
- High bleeding risk diseases
- Infections
- Electronic devices (pacemaker, etc.)
- Anatomical barriers
- Psychological issues
Surgery:
- Active infection
- Severe osteoporosis
- Severe cardiovascular problems
- Implant allergy
- Intolerance to certain biomaterials
Prolotherapy:
- Local abscess
- Bleeding issues
- Allergy to prolotherapy agents
- Acute fractures
- Acute gout arthritis
Patient history, including reactions to anesthesia or contrast agents and mental health conditions, should always be reviewed before intervention.
What Is the Recovery Process?
Recovery varies by treatment type. Minimally invasive surgery often allows for rapid return to daily life, but there is a 20% recurrence risk. Postoperative rehabilitation—starting within 4-6 weeks—accelerates tissue healing and functional recovery. In some cases (especially after ACDF), a cervical collar may be advised. Early and regular rehab is shown to improve outcomes and restore mobility.
How Can It Be Prevented?
- Regular exercise
- Strengthening core muscles
- Proper lifting techniques
- Maintaining a healthy weight
- Good ergonomic posture
- Avoiding smoking
- Regular stretching
- Avoiding prolonged inactivity
These measures protect the spine and help prevent disc herniation.
Patient Reviews of Lumbar Herniation Treatment
For patient reviews of Prof. Dr. Özgür Kılıçkesmez’s treatments, visit Google Maps or Doktortakvimi.
Frequently Asked Questions
How is nerve-compressing lumbar herniation diagnosed?
Diagnosis is based on clinical evaluation and imaging methods. MRI is the gold standard for visualizing the disc, nerves, and surrounding structures. If symptoms include loss of bladder or bowel control, seek emergency help.
What can be done at home to relieve symptoms?
Apply cold compresses for the first 48 hours, then switch to heat. Gentle walking and low-impact activities maintain mobility and strengthen muscles. Avoid long-term bed rest; use pain relievers like ibuprofen or paracetamol. Maintain correct posture and a healthy weight, quit smoking, and manage stress. Consult your doctor if symptoms persist or worsen.
How can herniation be managed before it progresses?
Physical therapy, medication, and lifestyle changes are essential. If conservative measures fail, epidural steroid injections or surgery may be considered. Early, personalized intervention offers the best outcomes.
When is physical therapy effective?
Physical therapy can reduce pain, improve function, and restore movement. Techniques such as mechanical traction, decompression, McKenzie exercises, and manual therapy are proven to help. Early rehab leads to better long-term results.

Interventional Radiology and Neuroradiology Speaclist Prof. Dr. Özgür Kılıçkesmez graduated from Cerrahpaşa Medical Faculty in 1997. He completed his specialization at Istanbul Education and Research Hospital. He received training in interventional radiology and oncology in London. He founded the interventional radiology department at Istanbul Çam and Sakura City Hospital and became a professor in 2020. He holds many international awards and certificates, has over 150 scientific publications, and has been cited more than 1500 times. He is currently working at Medicana Ataköy Hospital.







Vaka Örnekleri