Ehlers-Danlos syndrome (EDS) is a group of inherited connective tissue disorders affecting collagen synthesis. It is characterized by joint hypermobility, fragile skin, and vascular fragility, with severity varying across subtypes.
Joint symptoms include frequent dislocations, chronic pain, and instability. These complications significantly affect mobility and quality of life, often requiring long-term physiotherapy and supportive treatment.
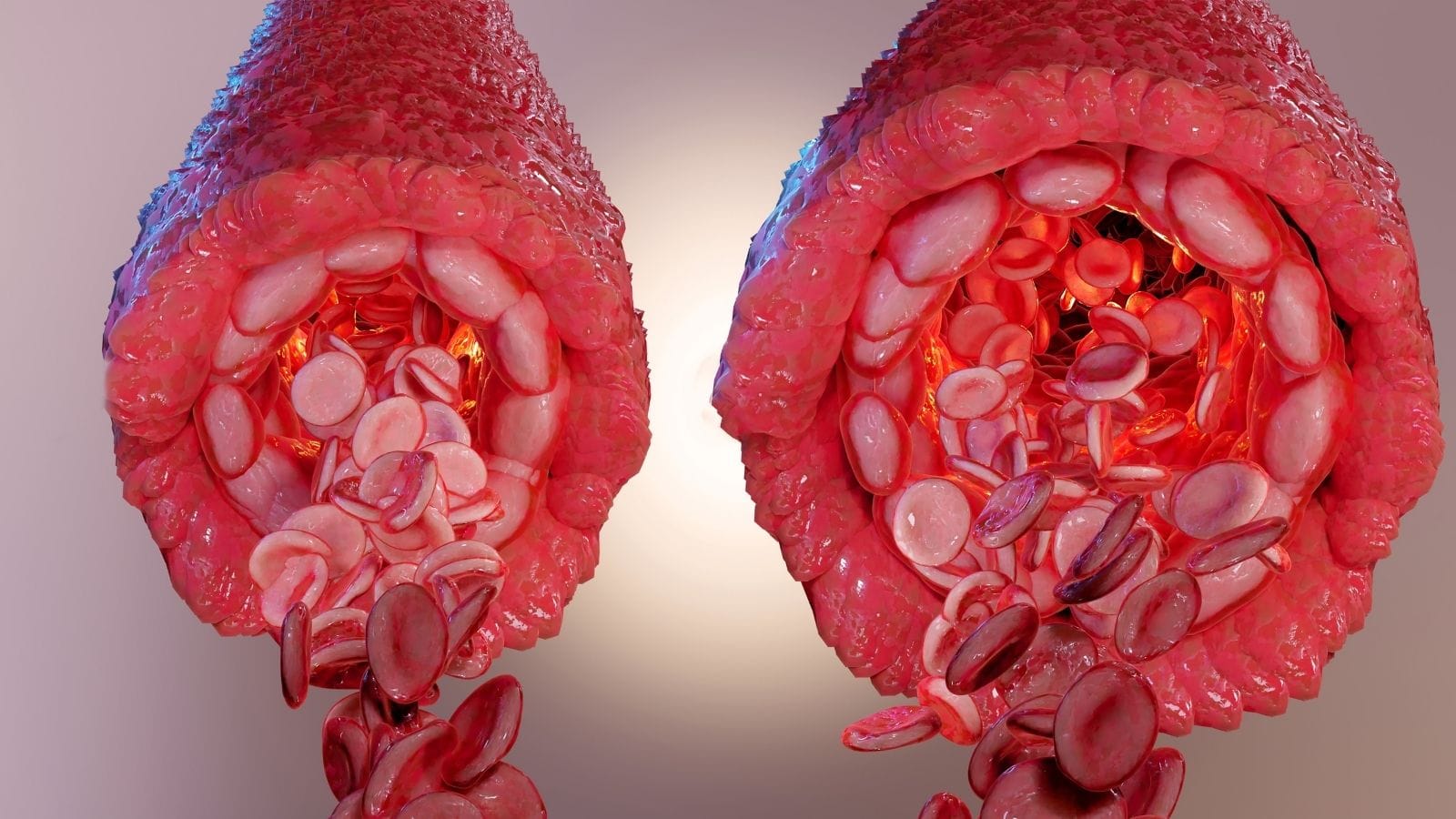
Vascular EDS is the most serious form, leading to arterial rupture, organ perforation, and life-threatening complications. Early diagnosis with genetic testing and regular monitoring is essential in high-risk patients.
Management focuses on symptom control and complication prevention. Multidisciplinary care involving physiotherapy, cardiology, and genetics helps patients maintain stability and reduce health risks.
| Disease Name | Ehlers-Danlos Syndrome (EDS) |
| Definition | A group of hereditary disorders caused by genetic defects in connective tissue, leading to elasticity and fragility in the skin, joints, and blood vessels. |
| Symptoms | Joint hypermobility (greater than normal flexibility), excessive skin elasticity and sensitivity, easy bruising, skin tears and poor healing, chronic pain, vascular ruptures in some types. |
| EDS Types | Classical Type, Hypermobile Type, Vascular Type, Kyphoscoliotic Type, Arthrochalasia Type, and Dermatospraxis Type; each type has different symptoms and genetic distinctions. |
| Causes | Mostly autosomal dominant inherited genetic mutations; the most common gene mutations are COL5A1, COL5A2, and COL3A1. The vascular type may cause more severe vascular problems. |
| Risk Factors | Genetic predisposition; individuals with a family history of EDS are at higher risk. |
| Diagnostic Methods | Physical examination, assessment of skin and joint flexibility, genetic tests (for definitive diagnosis), skin biopsy in certain cases. |
| Treatment Methods | Symptomatic treatment: physical therapy for joint stabilization, pain management, skin care for injuries; surgical intervention in severe cases (however, healing may be slow), cardiology follow-up for vascular issues. |
| Complications | Joint dislocations, chronic joint pain, non-healing skin wounds, vascular ruptures (life-threatening bleeding in vascular type), internal organ ruptures. |
| Surgical Requirement | If there are recurrent dislocations or weakness in the joints, surgical intervention may be necessary, but the healing process may be slow and complication risk is high. |
| Lifestyle Recommendations | Avoiding heavy lifting to prevent injuries, strengthening muscles with regular exercise, using protective clothing for joints, taking care of the skin, and remaining under medical supervision. |
| Genetic Counseling | Genetic counseling is recommended for those with a family history of EDS or after diagnosis; genetic testing and risk assessment can be performed before having children. |
Prof. Dr. Özgür KILIÇKESMEZ Prof. Dr. Kılıçkesmez holds the Turkish Radiology Competency Certificate, the Turkish Interventional Radiology Competency Certificate, Stroke Treatment Certification, and the European Board of Interventional Radiology (EBIR). In his academic career, he won the Siemens Radiology First Prize in 2008.
Interventional Radiology / Interventional Neuroradiology
What is Ehlers-Danlos Syndrome?
Ehlers-Danlos Syndrome (EDS) is a group of inherited connective tissue disorders affecting the skin, joints, blood vessels, and organs. This syndrome, which arises especially due to defects in collagen, disrupts the structural integrity of connective tissue. Associated with different genetic mutations, EDS is classified into 13 subtypes. Symptoms range from mild joint pain to life-threatening complications such as vascular ruptures. The main features of EDS include joint hypermobility, skin hyperextensibility, and tissue fragility. Most subtypes can be diagnosed by genetic tests. However, the genetic cause of hypermobile EDS has not yet been identified, making diagnosis difficult.
What Are the Causes of Ehlers-Danlos Syndrome?
Ehlers-Danlos Syndrome (EDS) arises from the effects of genetic mutations on connective tissue and encompasses many subtypes. Although each subtype is associated with specific genetic abnormalities, these mutations generally affect the structure of collagen proteins, leading to connective tissue weakness. EDS is mostly inherited in an autosomal dominant manner, but some rare types may show recessive inheritance.
- Collagen Mutations: Some types of EDS are associated with mutations in collagen genes. Classical EDS is due to mutations in the COL5A1 and COL5A2 genes, leading to impaired collagen production. This causes weakness in the skin and joint tissues. Vascular EDS is caused by mutations in the COL3A1 gene, which disrupts the structural integrity of blood vessels and increases the risk of rupture.
- Other Genetic Factors: EDS is not limited to collagen genes; other genes also play a role. For example, the TNXB gene associated with hypermobile EDS type affects connective tissue integrity. Also, the B3GALT6 gene is associated with the kyphoscoliotic EDS type and affects glycosaminoglycan (GAG) metabolism.
- Genetic Complexity and Environmental Factors: There is significant genetic diversity among EDS types, and especially the genetic basis of hypermobile EDS is not fully defined. Environmental factors can also affect the severity of symptoms, but research on this topic is still ongoing.
How Common Is Ehlers-Danlos Syndrome?
The prevalence of Ehlers-Danlos Syndrome (EDS) varies significantly among its subtypes. Considering all types together, it is estimated to affect approximately 1 in 5,000 people. However, it may be difficult to determine the exact prevalence for hypermobile EDS (hEDS), due to the ongoing development of diagnostic criteria. EDS cases are observed more frequently in women than men. However, this difference may reflect biases in the diagnostic process rather than a true prevalence rate. Symptoms can be seen at any age but become more apparent during childhood or adolescence.
EDS is a disorder that can occur in all ethnic groups, and some EDS types are reported more frequently in certain populations. Non-Caucasian individuals may have a higher likelihood of certain EDS types. However, the lack of available data for different ethnic groups limits this information.
Among EDS subtypes, there are common types with distinct characteristics:
- Hypermobile EDS (hEDS): Characterized by joint hypermobility and chronic pain.
- Classical EDS: Includes joint hypermobility with skin hyperextensibility and fragility.
- Vascular EDS: Poses a risk of severe complications due to blood vessel fragility.
- Kyphoscoliotic EDS and Dermatosparaxis EDS: Rare types based on specific genetic mutations.
The prevalence, clinical features, and risks of EDS types vary depending on these characteristics.
*We recommend filling out all fields so we can respond in the best possible way.
How Does Ehlers-Danlos Syndrome Develop?
The development process of Ehlers-Danlos Syndrome (EDS) becomes distinct through genetic mutations and structural abnormalities of connective tissue. The subtypes of EDS mainly arise from defects in collagen and other extracellular matrix proteins. These genetic mutations cause problems in the structure, resilience, and function of connective tissue, leading to various clinical symptoms.
Genetic mutations in EDS are usually transmitted via autosomal dominant or autosomal recessive inheritance. However, some mutations occur de novo, developing spontaneously during embryonic development. This is explained by the appearance of new mutations in a child not seen in the parents. Collagen is the main protein affected by genetic disorders; the structural integrity of collagen determines the resistance of connective tissue.
The genetically defined subtypes of EDS are as follows:
- Classical EDS: Characterized by skin elasticity, easy bruising, and abnormal scars.
- Hypermobile EDS (hEDS): Defined by joint hypermobility; no genetic mutation has been identified.
- Vascular EDS: Involves blood vessel fragility and the risk of arterial rupture.
Collagen defects result in connective tissue weakness, leading to symptoms such as joint hypermobility, easy bruising, and slow wound healing. Due to mutations, connective tissue loses its resistance, increasing susceptibility to damage.
What Are the Symptoms of Ehlers-Danlos Syndrome?
Ehlers-Danlos Syndrome presents with various symptoms due to abnormalities in the body’s connective tissue. Prominent symptoms of this syndrome include joint hypermobility, chronic pain, and skin abnormalities. In addition, some EDS types can involve cardiovascular and neurological problems. The symptoms are as follows:
- Joint Hypermobility: Unusually flexible joints, frequent dislocations, and subluxations.
- Chronic Pain: Characterized by persistent joint, muscle, and musculoskeletal pain.
- Skin Abnormalities: Symptoms such as skin elasticity, fragility, and easy bruising.
- Cardiovascular Problems: Fragile blood vessels and mitral valve prolapse may be observed in some subtypes.
- Neurological Symptoms: Problems such as numbness, migraines, and nerve entrapment may occur.
- Organ Prolapse: Seen as displacement of digestive or reproductive organs.
- Developmental Delay: Delayed development of motor skills and hypotonia can be observed.
How Is Ehlers-Danlos Syndrome Diagnosed?
The diagnosis of Ehlers-Danlos Syndrome involves a detailed physical examination, genetic tests, and sometimes special imaging techniques. The process usually begins by evaluating characteristic features such as joint hypermobility, skin hyperextensibility, and tissue fragility. Since EDS is a genetic disorder, family history plays a critical role in diagnosis.
Clinical Criteria:
- Physicians assess joint hypermobility and skin hyperextensibility using tools such as the Beighton score.
- The elasticity of certain skin areas can be measured with hyperextensible skin, which shows abnormally increased stretchability.
- Hypermobile joints with exaggerated range of motion are important diagnostic indicators.
- Additional features include “cigarette paper”-like scars and poor wound healing.
Genetic Testing:
- Genetic tests are important to distinguish the 13 subtypes of EDS and confirm the diagnosis.
- Blood samples can detect mutations in genes responsible for collagen and connective tissue abnormalities.
- However, not all types of EDS have identifiable genetic markers; especially hypermobile EDS (hEDS) is unclear in this regard.
Skin Biopsy and Imaging:
- For classical or vascular EDS types, a skin biopsy may be taken to examine collagen structure.
- Echocardiography and vascular ultrasounds are used, especially for detecting vascular complications.
Additional Tests:
- MRI and CT scans are preferred to evaluate joint and spinal abnormalities.
- Imaging helps determine serious conditions such as arterial rupture in severe vascular EDS forms.
How Is Ehlers-Danlos Syndrome Treated?
In Ehlers-Danlos Syndrome (EDS), especially in the vascular subtype (vEDS), interventional radiology plays an important role in the treatment of vascular complications. vEDS causes life-threatening vascular problems such as aneurysm, arterial dissection, and rupture due to arterial fragility. Since traditional surgical interventions carry high risks in such cases, minimally invasive methods provide a safer and more appropriate approach. In this context, endovascular procedures are preferred to manage treatment processes for patients.
The main endovascular procedures applied in treatment are as follows:
- Embolization: This method, effective in controlling arterial bleeding, is used in emergencies to stop life-threatening hemorrhages.
- Stent Grafting: Assists in repairing vessels in cases such as pseudoaneurysm and arterial dissection. Provides safer protection, especially for patients with fragile vessel structures.
- Coil Embolization: Used in aneurysm treatment to control blood flow and prevent vascular ruptures.
The application of minimally invasive methods in vEDS patients brings some challenges due to vascular fragility. Complications such as vascular perforation or dissection may occur during catheterization in these patients. Therefore, it is important that treatment processes are managed by a multidisciplinary team including experienced interventional radiologists. Endovascular treatments performed by experienced teams show successful results in the management of aneurysms and other acute vascular problems.
What Are the Risk Factors for Ehlers-Danlos Syndrome?
Ehlers-Danlos Syndrome (EDS) is a connective tissue disorder developed due to genetic mutations and is associated with specific risk factors. The main risk factors for EDS are family history, genetic mutations, and gene-environment interactions. Individuals with a family history of EDS have a higher risk, as EDS is usually inherited in an autosomal dominant manner from parent to child.
Genetic mutations disrupt the structure of collagen, a main component of connective tissue, leading to different EDS subtypes. Especially mutations in genes such as COL5A1, COL5A2, and COL3A1 affect collagen synthesis. This results in prominent EDS symptoms such as joint hypermobility, skin fragility, and vascular complications.
Another risk factor for EDS is gene-environment interactions. Although it is a genetic disorder, environmental factors can increase the severity of symptoms. For example, physical strain or trauma can worsen symptoms in genetically predisposed individuals. This can make the disease more apparent and increase the risk of complications.
Finally, some EDS subtypes show higher prevalence in women. While the exact reasons for this are not fully understood, it may be associated with hormonal effects or differences in joint structure between genders.
When Can Ehlers-Danlos Syndrome Be Treated?
In Ehlers-Danlos Syndrome, especially in the vascular type (vEDS), serious vascular complications make correct timing of treatment critical. These patients frequently experience arterial ruptures, aneurysms, dissections, and pseudoaneurysms, which can lead to life-threatening bleeding. Due to the fragility of vascular structures, interventional radiological methods are primarily used to minimize surgical risks and control complications. However, various factors should be considered when determining appropriate treatment timing.
The main indications are:
- Arterial Ruptures or Aneurysms: Patients with vEDS are at high risk for spontaneous arterial ruptures and aneurysms. The management of these lesions is urgent, especially to prevent sudden hemorrhage.
- Dissections and Pseudoaneurysms: Arterial dissections and pseudoaneurysms can cause severe blood loss. When ruptured vessels need to be closed, transcatheter embolization is preferred before surgical intervention.
Preventive interventions may also be important in some cases. If rapidly growing aneurysms or vessels prone to dissection are detected on imaging, preventive treatments can be planned. Especially in high-risk patients, the best results may be achieved by combining limited surgical approaches with endovascular methods. These hybrid treatment methods help improve patient quality of life and prevent more serious complications. The timing of treatment is determined by considering existing risk factors and the condition of the vascular structures.
When Can Ehlers-Danlos Syndrome Not Be Treated?
In patients with Ehlers-Danlos syndrome, especially the vascular subtype (vEDS), interventional radiology methods must be evaluated with caution due to some serious contraindications. The fragility of the vessels increases the potential risks of such interventions, making many procedures contraindicated. Especially structural weaknesses in the vessels can cause a high risk of complications during invasive procedures. Vascular fragility in vEDS patients is an important factor to consider during invasive procedures, carrying the following risks:
- Vascular Fragility: Fragility in the vessels can lead to spontaneous arterial ruptures and dissections in vEDS patients. Invasive procedures such as catheter placement can cause vascular ruptures.
- High Morbidity and Mortality Rates: Diagnostic angiography and therapeutic interventions carry high morbidity and mortality risks in these patients. Diagnostic procedures may have a 35% morbidity rate and interventional treatments a 12% mortality rate.
- Avoiding High-Pressure Injections: Procedures such as power injection apply high pressure to arterial walls, increasing the risk of vascular rupture and leading to dangerous outcomes.
- Stent Placement and Embolization Challenges: Due to structural weaknesses, vessel walls may not provide support during stent placement, and complications such as stent migration may occur.
What Is the Recovery Process After Ehlers-Danlos Syndrome Treatment?
The recovery process after treatment for Ehlers-Danlos Syndrome (EDS) is particularly complex and needs to be managed carefully in vascular EDS (vEDS) patients. In the first days after surgery, patients are closely monitored in the intensive care unit for hemodynamic observation. Due to the risks of vascular ruptures, embolic events, or new dissections, careful follow-up is essential. Patients require continuous observation during the recovery process, and regular imaging is performed for early detection of potential complications. Risks such as recurrent bleeding, pseudoaneurysm formation, and thrombosis are evaluated during this process.
Even with successful treatment, vascular complications may persist in the postoperative period. Non-invasive methods are generally preferred to reduce risks. The recovery process, managed by a multidisciplinary team, is shaped according to the individual’s genetic profile and previous treatments.
During recovery, patients are given drug therapy and are advised to avoid certain activities:
- Drug Therapy: Beta blockers are frequently preferred, especially for their stress-reducing effect on the vessel wall.
- Activity Restrictions: Physical activities are limited and monitored to prevent vascular strain.
Regular imaging during the recovery process is important for the early detection of complications. During the ongoing recovery period, repeat interventional radiology procedures may be necessary to prevent aneurysm expansion or new dissections. Long-term management, lifestyle changes, and regular follow-ups help keep the patient’s condition under control.
How Can Ehlers-Danlos Syndrome Be Prevented?
Since Ehlers-Danlos Syndrome (EDS) is a genetic disorder, preventive approaches aim not to eliminate the disease itself but to reduce complications. While the intergenerational transmission of EDS cannot be stopped, there are some ways to improve patients’ quality of life. Prevention strategies focus on genetic counseling, prevention of complications, and management of symptoms.
- Genetic Counseling: Genetic counseling is highly important for individuals and families with a history of EDS. This process helps parents understand the risks of transmission to their children. Especially for severe types such as vascular EDS, prenatal genetic tests can be offered as an option. Conscious reproductive choices can thus be made.
- Prevention of Complications: Certain adaptations should be made in the daily lives of people with EDS. High-impact activities should be avoided to protect joint health, and physical therapy methods should be applied. Low-impact exercises and the use of supportive devices increase joint stability and help prevent dislocations. In riskier cases such as vascular EDS, regular cardiovascular monitoring and medical treatment can protect vascular health.
- Medical Management of Symptoms: Physiotherapy and occupational therapy can help manage symptoms such as pain and fatigue. In addition, chronic pain management and treatments for gastrointestinal problems can improve patients’ quality of life.
Research to resolve the molecular causes of EDS is ongoing, which may pave the way for new treatments in the future.

Girişimsel Radyoloji ve Nöroradyoloji Uzmanı Prof. Dr. Özgür Kılıçkesmez, 1997 yılında Cerrahpaşa Tıp Fakültesi’nden mezun oldu. Uzmanlık eğitimini İstanbul Eğitim ve Araştırma Hastanesi’nde tamamladı. Londra’da girişimsel radyoloji ve onkoloji alanında eğitim aldı. İstanbul Çam ve Sakura Şehir Hastanesi’nde girişimsel radyoloji bölümünü kurdu ve 2020 yılında profesör oldu. Çok sayıda uluslararası ödül ve sertifikaya sahip olan Kılıçkesmez’in 150’den fazla bilimsel yayını bulunmakta ve 1500’den fazla atıf almıştır. Halen Medicana Ataköy Hastanesi’nde görev yapmaktadır.







Vaka Örnekleri